Understanding why we burp babies is not just a tradition passed from one generation to another, but a medically supported practice that plays a vital role in newborn care. For new moms navigating the uncharted territory of maternity, this often-overlooked habit is more than a comforting routine—it is a key strategy for reducing infant discomfort, preventing feeding complications, and supporting digestive health. This guide explores the physiological, emotional, and practical reasons behind burping, offering deep insights that will help demystify the process and empower parents to nurture their babies with confidence and care.
You may also like: Essential Baby Care and Maternity Tips Every First Time Parent Needs to Know
The Science Behind Infant Digestion
Newborns enter the world with immature digestive systems that require support and patience to develop. Unlike older children and adults, who have the muscle coordination to regulate and expel internal gas effectively, babies rely on external help to release swallowed air during feeding. When infants breastfeed or bottle-feed, they inevitably swallow air, particularly if they latch improperly, feed too quickly, or cry during mealtime. This trapped air can accumulate in the stomach, causing pressure, bloating, and discomfort that often manifest as fussiness, crying, or interrupted sleep.
Burping serves as a pressure-release mechanism that helps infants eliminate this excess air. By gently patting or rubbing the baby’s back while holding them upright, parents can stimulate the release of gas through the esophagus and out of the mouth. This process, while seemingly simple, can significantly improve the baby’s comfort and overall feeding experience. Understanding this physiological response underscores why burping is not optional, but essential for promoting a smoother digestive transition from womb to world.

Why Do We Burp Babies: The Critical Connection Between Air Intake and Discomfort
Why do we burp babies? The answer lies in a combination of anatomy, feeding mechanics, and developmental needs. Infants have an underdeveloped lower esophageal sphincter (LES), the muscle that separates the esophagus from the stomach. A weak LES makes it easier for air and stomach contents to travel back up the esophagus, leading to reflux and spit-up episodes. By proactively burping a baby after feeding, caregivers can reduce the amount of air trapped in the stomach, lowering the risk of reflux and minimizing discomfort.
Additionally, the shape and positioning of a baby’s body during feeding can contribute to the volume of air swallowed. Bottle-fed babies, for example, are more likely to ingest air if the bottle is tilted incorrectly or if the nipple does not remain filled with milk. Breastfed babies may swallow air due to a shallow latch or changes in milk flow. Regardless of the feeding method, burping serves as a proactive measure to address the root causes of discomfort, making it a vital practice for both short-term relief and long-term digestive health.
Positions for Burping a Newborn: Maximizing Comfort and Effectiveness
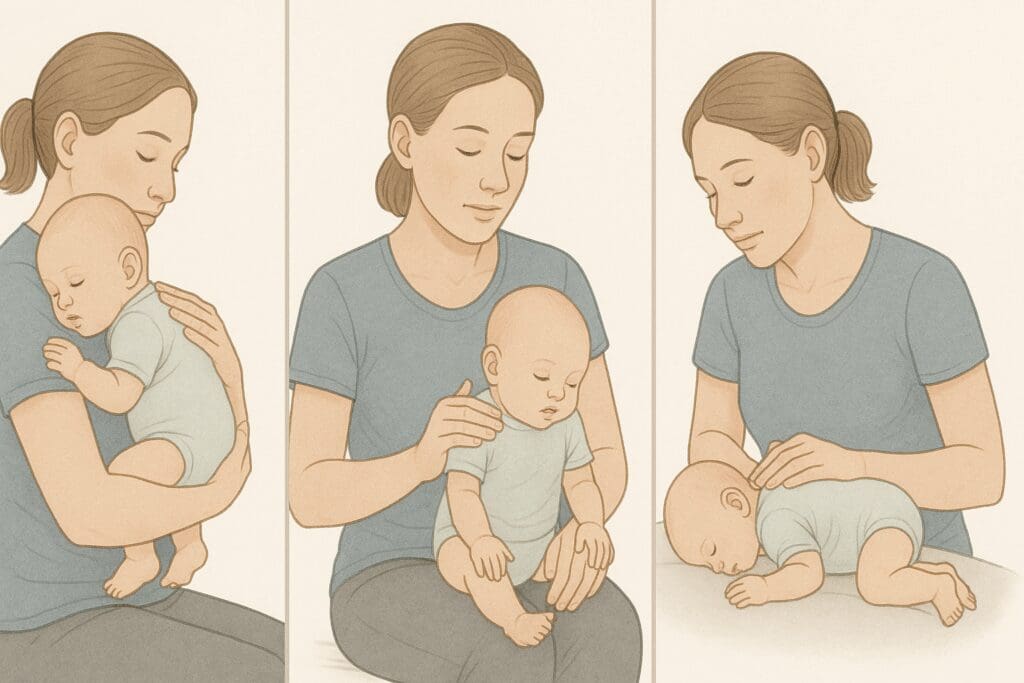
The effectiveness of burping largely depends on positioning. Various positions can help maximize gas release while keeping both the baby and caregiver comfortable. Among the most recommended is the over-the-shoulder position, where the baby rests upright with their head on the caregiver’s shoulder, allowing gravity to assist in the upward movement of trapped air. In this position, gentle pats or circular rubs on the back help stimulate the burping reflex.
Another effective method involves sitting the baby on the caregiver’s lap with one hand supporting the chest and head, while the other gently pats the back. This upright position not only facilitates gas expulsion but also allows the caregiver to observe any signs of discomfort or reflux. A third option is laying the baby face-down across the lap, with the head slightly elevated. This prone position applies gentle pressure to the stomach, which can assist in releasing trapped air.
Each baby is unique, and what works for one may not work for another. New parents are encouraged to experiment with different positions to determine which one yields the best results. Importantly, all burping positions should prioritize the baby’s head and neck support, ensuring safety and comfort throughout the process.

How to Properly Burp a Newborn Without Disrupting Sleep
A common challenge new parents face is learning how to properly burp a newborn without waking them, especially during nighttime feedings. Many babies fall asleep while nursing or bottle-feeding, and the idea of disrupting their rest can make parents hesitant to attempt burping. However, skipping this step may lead to interrupted sleep later, as gas buildup can cause discomfort that rouses the baby.
The key to a gentle, sleep-friendly burping technique lies in maintaining a calm environment and using soft, rhythmic motions. Instead of vigorous pats, a light rub in an upward circular motion can often be enough to elicit a burp without startling the baby. Supporting the baby in an upright position against the caregiver’s chest allows gravity to work naturally, minimizing the need for additional stimulation.
It is also helpful to pay attention to signs of partial arousal. If a baby shifts or squirms slightly during sleep, it may indicate the presence of trapped gas. In such cases, a gentle attempt to burp without fully waking the baby can be both effective and nurturing. This approach requires patience, but it can result in longer, more restful sleep periods for both the infant and the caregiver.
The Best Way to Burp an Infant: Expert Tips and Real-World Insights
While there is no one-size-fits-all approach, understanding the best way to burp an infant involves a combination of technique, timing, and observation. Timing is especially crucial; most pediatricians recommend burping a baby midway through feeding as well as after the session ends. This dual approach helps manage air intake during feeding and prevents the buildup of discomfort after the meal.
In terms of technique, the goal is to use firm yet gentle pressure to stimulate the diaphragm and esophagus. Some babies respond best to patting, while others may prefer a rubbing motion. Observing the baby’s response can guide caregivers in fine-tuning their approach. Additionally, using tools such as burp cloths, bibs, and appropriate seating can help create a comfortable routine for both the baby and the parent.
Real-world insights from experienced parents often highlight the importance of patience and intuition. Babies may not burp immediately, and it can take several minutes for the gas to rise. Remaining calm and persistent without applying excessive force is key. Recognizing the signs of successful burping—a small belch, a sudden sigh, or a relaxed body posture—helps build confidence and fosters a positive feeding experience.
Why Do We Burp Babies: Preventing Colic, Reflux, and Fussiness
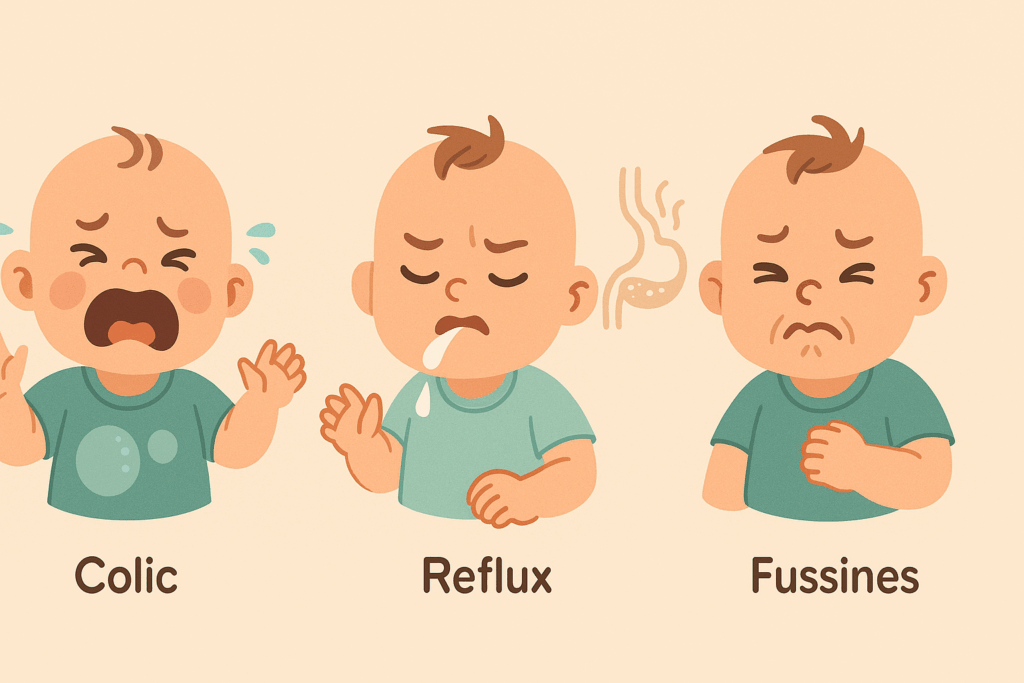
Returning to the central question—why do we burp babies?—it becomes clear that burping is more than just an optional ritual. It plays a direct role in preventing a range of feeding-related issues, including colic, reflux, and general fussiness. Colic, characterized by prolonged crying spells and apparent abdominal discomfort, remains a poorly understood but highly distressing condition. Many experts believe that trapped gas exacerbates colic symptoms, making burping a key intervention for symptom relief.
Reflux, or gastroesophageal reflux (GER), is another common concern among newborns. When air and stomach contents move back up the esophagus, they can cause pain, regurgitation, and feeding aversion. Burping minimizes the volume of air in the stomach, thereby reducing the likelihood of reflux episodes. This preventative effect is particularly beneficial for babies who feed frequently or have existing gastrointestinal sensitivities.
Beyond the physical benefits, burping also supports emotional regulation. Babies who are less gassy tend to be more content, easier to soothe, and better able to engage in eye contact and bonding. By alleviating the physical discomfort associated with feeding, burping enhances the overall caregiving experience, promoting a more harmonious start to life.
The Evolution of Burping Practices: Cultural and Historical Perspectives
Burping has been a staple of infant care across cultures and centuries, though the methods and beliefs surrounding it vary widely. In some cultures, burping is considered essential immediately after feeding, while in others, the emphasis is placed more on positioning and timing rather than the act itself. Historical records suggest that burping practices were passed down orally, rooted in maternal instinct and community wisdom.
Modern science has validated many of these practices, shedding light on the underlying physiological mechanisms that make burping effective. For instance, the increased prevalence of bottle-feeding in industrialized nations has drawn attention to the importance of managing air intake, making burping a more central focus in contemporary parenting guides. Meanwhile, traditional societies that emphasize extended breastfeeding may approach burping with greater flexibility, relying on body positioning and baby-wearing techniques to achieve the same effect.
Understanding the cultural diversity of burping practices enriches the parenting journey. It empowers caregivers to draw from a wide array of strategies, blending modern medicine with timeless wisdom. This inclusive perspective fosters empathy, flexibility, and resilience in the ever-evolving landscape of early childhood care.
How to Properly Burp a Newborn: Avoiding Common Mistakes
Even the most well-intentioned parents can struggle with burping, especially when navigating sleepless nights and fluctuating feeding schedules. One common mistake is assuming that if a baby doesn’t burp within a few seconds, no air is present. In reality, gas can take time to surface, and premature cessation of burping attempts may leave the baby uncomfortable.
Another frequent error involves improper positioning. Failing to support the baby’s head and neck adequately can not only reduce the effectiveness of burping but also increase the risk of injury. Likewise, using excessive force or overly vigorous patting may startle the baby and create negative associations with feeding.
To avoid these pitfalls, caregivers should focus on gentle consistency. Establishing a calm, predictable routine around feeding and burping helps both the baby and parent stay attuned to one another. Incorporating breaks during feeding to check for signs of discomfort, using well-padded burp cloths, and experimenting with different positions can all contribute to a more successful and satisfying experience.
Why Do We Burp Babies: The Emotional and Developmental Payoff
The question “why do we burp babies” also invites a deeper reflection on the emotional dimensions of infant care. Burping is not just about removing air; it is a moment of closeness, communication, and comfort. When a caregiver holds a baby upright, supports their body, and patiently soothes them through the process, they are building a foundation of trust and security that has far-reaching developmental implications.
This physical closeness activates oxytocin release in both the baby and the parent, reinforcing bonding and reducing stress. The act of burping becomes a ritual of attentiveness, where subtle cues are exchanged and interpreted. Over time, this responsiveness nurtures emotional intelligence, self-regulation, and attachment security in the growing child.
Moreover, consistent burping routines help establish predictable caregiving patterns, which are essential for cognitive and emotional development. Babies thrive on consistency, and the predictability of being burped after each feeding session reinforces a sense of order and safety. In this way, burping contributes to the larger tapestry of nurturing care that supports holistic development during the critical early months of life.
When to Seek Medical Advice: Recognizing Abnormal Symptoms
While burping is a generally straightforward and benign practice, there are times when excessive gas, frequent spit-up, or unusual discomfort may indicate an underlying medical condition. Parents should be aware of signs that suggest the need for professional evaluation, such as persistent vomiting, failure to gain weight, chronic irritability, or refusal to feed. These symptoms may point to conditions like gastroesophageal reflux disease (GERD), food allergies, or anatomical abnormalities that require targeted interventions.
A pediatrician can conduct a thorough assessment and provide guidance tailored to the baby’s individual needs. This may include adjustments to feeding techniques, changes in diet for breastfeeding mothers, or the introduction of specialized formulas. In some cases, further diagnostic testing may be warranted to rule out more serious gastrointestinal issues.
The takeaway is that while burping is highly effective in most scenarios, it is not a panacea. Being attuned to the baby’s unique patterns and seeking timely medical input when needed ensures that caregivers can provide the most informed and supportive care possible.
Frequently Asked Questions: Expert Insights Into Why Do We Burp Babies and Infant Care
Why do we burp babies after every feeding, even if they seem content?
Many parents assume that if a baby appears calm after feeding, there’s no need to burp. However, the absence of immediate discomfort doesn’t always mean the absence of swallowed air. Infants can accumulate small air pockets that slowly build up and create discomfort later, often leading to restlessness during sleep. Burping after each feeding, even when a baby seems fine, acts as a preventive measure. It helps avoid delayed symptoms like night waking, spit-up, or abdominal tension that might otherwise go unnoticed. By prioritizing post-feeding burping, caregivers can ensure the baby digests more efficiently and stays comfortable longer, reducing disruptions in feeding and sleeping cycles.
How can I identify the best way to burp infant twins when feeding them together?
Burping twins can be uniquely challenging due to the logistics of feeding two infants simultaneously. The best way to burp infant twins often involves alternating feeding and burping instead of feeding both entirely before attempting to burp them. One effective approach is to burp the first twin midway through their feed, set them safely in a semi-upright position, and then begin feeding the second twin. This rotational method prevents either baby from accumulating too much air. Some parents also find success using twin feeding pillows that allow both babies to stay in slightly elevated positions, making transitions between feeding and burping smoother. Developing a consistent sequence that accommodates both babies’ digestion rhythms is key to ensuring optimal comfort and reducing gas-related fussiness.
What are some underused positions for burping a newborn that offer high success rates?
Beyond the typical over-the-shoulder and lap-sitting techniques, a few lesser-known positions for burping a newborn can yield excellent results. One such method involves holding the baby in a football hold—facing outward, with the baby’s stomach supported along the caregiver’s forearm and head secured in the hand. This position not only promotes gas release but also frees the caregiver’s other hand to gently pat or massage the baby’s back. Another effective but often overlooked position is laying the baby on their tummy across the caregiver’s thighs while gently bouncing the legs in a slow rhythm. This motion, combined with light back pressure, can coax out stubborn gas bubbles. Exploring different positions can be especially helpful for babies with colic or reflux, where standard burping techniques may fall short.
Why do we burp babies during dream feeds, and is it really necessary?
Dream feeds—when parents feed babies without fully waking them—are a popular method to extend overnight sleep. However, many parents wonder whether interrupting this calm moment for burping is necessary. The answer lies in understanding how newborns’ digestion works even during semi-conscious states. During a dream feed, the baby still swallows milk and, inevitably, air. Skipping the burping step can lead to gas accumulation that surfaces later in the form of disrupted sleep or discomfort. Even a gentle hold in an upright position for a few minutes can allow gravity to help naturally release trapped air without fully waking the baby. For dream feeding to truly work as intended, incorporating a quiet, minimally disruptive burping routine is a wise and proactive measure.
How do I adapt the best way to burp infant babies with special needs or developmental delays?
Burping babies with developmental delays or specific medical conditions requires extra care and customization. These infants may experience hypotonia (reduced muscle tone), which makes it harder for them to move swallowed air upward on their own. In such cases, the best way to burp infant children involves supporting their bodies in well-padded, upright positions for longer durations while using slow, rhythmic circular motions on their back. Additionally, caregivers may need to consult with pediatric physical therapists to learn modified handling techniques that support musculoskeletal and gastrointestinal needs simultaneously. Babies with feeding tubes or swallowing difficulties may not always show standard signs of gas discomfort, so scheduled burping intervals become more important. Always involve healthcare professionals when tailoring burping techniques for babies with additional medical considerations.
Why do we burp babies differently depending on bottle versus breast feeding?
The method of feeding can significantly influence how and when burping is most effective. Bottle-fed babies often swallow more air due to the artificial nipple’s structure and faster milk flow, especially if the bottle is tilted incorrectly or the nipple collapses. As a result, they may require more frequent and vigorous burping. On the other hand, breastfed infants typically take in less air, but issues like a shallow latch or overactive let-down can increase air intake. Therefore, understanding the dynamics of each feeding method helps caregivers decide on the timing and positions for burping a newborn. Some breastfed babies benefit from being burped only once, while bottle-fed babies may need pauses throughout the feeding. Observing each baby’s cues in context with how they are fed can fine-tune the caregiver’s strategy for better digestive comfort.
Can the best way to burp infant babies change as they grow older?
Absolutely. As babies develop, their digestive systems and muscular strength mature, altering their burping needs and responsiveness. Newborns under three months typically require consistent burping because they have weaker diaphragms and lower esophageal sphincters. However, by four to six months, many infants begin to outgrow the need for frequent burping, especially if they can sit upright with minimal support. That said, growth spurts or the introduction of solid foods may temporarily bring back episodes of gas buildup, necessitating occasional burping even in older babies. The best way to burp infant children at different ages will also evolve, shifting from fully supported positions to more active participation from the baby. Paying attention to developmental milestones can help caregivers adjust burping routines to align with their child’s physical readiness and comfort needs.
Why do we burp babies in specific positions, and how does body posture influence burp success?
Body posture plays a surprisingly critical role in how efficiently air can escape from the baby’s stomach. The upright position facilitates the natural ascent of gas bubbles by aligning the esophagus vertically and reducing pressure on the stomach. For instance, in the over-the-shoulder method, gravity assists in pulling gas upward, especially when combined with soothing back pats. The sitting position, where the baby is propped on the lap, allows gentle spinal extension, which opens up the diaphragm and promotes easier air movement. Alternatively, semi-inclined or tummy-down positions apply subtle pressure to the abdomen, aiding burp release by compressing the stomach in a controlled way. Understanding the physiological mechanics behind various positions for burping a newborn allows parents to rotate techniques based on feeding context, time of day, or the baby’s temperament.
How does parental stress impact the effectiveness of how to properly burp a newborn?
While often overlooked, caregiver stress can directly affect how to properly burp a newborn. When parents are anxious or fatigued, their touch may become less coordinated or more forceful, which can startle a baby or reduce burping efficiency. Infants are highly sensitive to their caregiver’s emotional state, and heightened tension during feeding can lead to a more restless experience for both parties. Practicing mindful burping—where caregivers center themselves, breathe deeply, and focus fully on their baby—can help establish a calm and effective routine. Even small adjustments like soft background music, dim lighting, or a soothing tone of voice can make the process more relaxing and productive. Recognizing the bi-directional emotional connection in caregiving situations is vital for success in feeding and burping, especially during challenging developmental phases.
Why do we burp babies in public settings, and how can caregivers navigate it with confidence?
Feeding and burping on the go can feel daunting, especially for new parents concerned about privacy, mess, or public perception. However, learning to burp in public settings becomes essential as social activities and errands resume postpartum. Portable burp cloths, discreet baby wraps, and knowledge of effective positions for burping a newborn can empower parents to manage burping needs confidently in cafes, airports, or parks. For instance, sitting upright with the baby in a burp-ready posture against the caregiver’s chest can be both subtle and effective. Choosing quieter moments during an outing and being prepared with extra clothing or wipes helps reduce anxiety. Ultimately, normalizing the conversation around infant care in public helps break down stigma and supports a healthier, more informed parenting culture for everyone involved.
Final Thoughts: Why Burping Babies Is a Vital, Science-Backed Act of Love
Burping may seem like a small detail in the vast landscape of newborn care, but it carries profound implications for a baby’s comfort, health, and development. Understanding why we burp babies helps new parents appreciate the importance of this simple yet powerful practice. From preventing digestive discomfort to enhancing emotional bonds and supporting sleep quality, burping emerges as a cornerstone of early caregiving.
Incorporating expert-backed techniques, such as identifying the best way to burp an infant or mastering positions for burping a newborn, elevates this act from routine to ritual. Knowing how to properly burp a newborn not only safeguards against common issues like colic and reflux but also strengthens the caregiver-infant connection in meaningful ways. Each gentle pat, each soothing rub, becomes part of a broader narrative of nurturing, responsiveness, and love—laying the foundation for a lifetime of secure attachment and holistic well-being.



