Understanding the Right Time to Begin Hormone Support
The question of when to start hormone replacement therapy during menopause is more than a matter of timing—it is central to a woman’s overall health, longevity, and quality of life. Menopause, a natural biological transition that signifies the end of reproductive years, brings with it a cascade of hormonal fluctuations. These shifts can be subtle for some but debilitating for others, triggering symptoms ranging from insomnia and hot flashes to anxiety and bone loss. Hormone replacement therapy (HRT) offers a scientifically grounded intervention to help restore hormonal balance, but its timing significantly influences both its effectiveness and safety profile. This article explores the physiological, clinical, and personal considerations that define the ideal window for initiating hormone therapy, incorporating the latest research and a nuanced understanding of hormonal health.
Initiating HRT is not a one-size-fits-all decision. The body’s readiness, symptom severity, age at onset, and preexisting conditions all play a role. Recent discussions about the pros and cons of hormone therapy reflect a maturing field, one that has moved beyond fear-based generalizations. Today, women want answers: Is hormone replacement therapy safe? What are the benefits of HRT if started early? And, crucially, when is the ideal moment to begin treatment to ensure the best outcomes? These are not merely academic questions—they are deeply personal ones that deserve informed, evidence-based guidance.
In the sections that follow, we will demystify the mechanisms of HRT, address common myths, and provide concrete answers to the pivotal question: when to start hormone replacement therapy. By balancing clinical science with personal narrative and practical advice, we aim to illuminate the path toward empowered, hormone-informed living during menopause and beyond.
You may also like: The Essential Guide to Choosing the Right Diet for Menopause: What Every Woman Should Know

The Hormonal Architecture of Menopause
To understand the rationale behind HRT timing, it is essential to first examine the hormonal transformations that occur during menopause. Menopause is clinically defined as the cessation of menstrual periods for 12 consecutive months, typically occurring between the ages of 45 and 55. However, the transition can begin years earlier in a phase known as perimenopause, where estrogen and progesterone levels start to fluctuate erratically.
These hormonal changes affect every organ system. Estrogen, often viewed through the narrow lens of reproductive health, actually influences over 400 bodily functions. It plays a critical role in cardiovascular protection, bone density maintenance, skin elasticity, cognition, and even mood regulation. When estrogen levels drop, these systems become vulnerable, often giving rise to symptoms like joint pain, dry skin, irritability, and cognitive fog.
During perimenopause, the ovaries reduce their production of estrogen and progesterone, often in an inconsistent and unpredictable manner. This hormonal seesaw can lead to irregular periods, breast tenderness, and disrupted sleep. By the time menopause is officially reached, the body’s natural estrogen production has dwindled dramatically, often leaving women with symptoms that persist for years unless addressed. Understanding this hormonal timeline provides the biological framework for evaluating when to start hormone replacement therapy.
The “Timing Hypothesis”: Why Early Initiation Matters
One of the most significant advancements in menopause research has been the emergence of the “Timing Hypothesis,” a theory supported by extensive clinical data. According to this hypothesis, the benefits of HRT—especially the best estrogen replacement options—are most pronounced when therapy is initiated within a critical window, typically within ten years of menopause onset or before age 60.
Studies have shown that starting HRT during this window reduces the risk of cardiovascular disease, preserves cognitive function, and strengthens bones. When initiated early, hormone therapy appears to mimic the body’s natural hormonal rhythm, thereby optimizing physiological harmony and minimizing side effects. In contrast, starting HRT much later in life—particularly after age 70—may pose risks that outweigh the benefits, such as increased likelihood of stroke or thrombosis.
The concept of hormone replacement before and after this critical window has profound implications. For example, a woman who begins experiencing menopausal symptoms in her early 50s and delays treatment for a decade may find herself past the optimal initiation phase, limiting the effectiveness of therapy and increasing her risk profile. This underscores the urgency of answering the question: when to start hormone replacement therapy, especially for women who are navigating perimenopause or early menopause symptoms.
Evaluating Early Symptoms: Do I Need Hormone Replacement Therapy?
Many women find themselves asking, “Do I need hormone replacement therapy?” during the confusing early stages of perimenopause. This question often arises when symptoms begin to interfere with daily life—whether that’s trouble sleeping, unexpected weight gain, mood instability, or declining libido. While these symptoms are common, they are not inevitable, nor do they have to be endured without support.
The decision to start HRT is ideally made in collaboration with a healthcare provider who specializes in hormonal health. Blood tests may provide baseline data about estrogen, progesterone, and follicle-stimulating hormone (FSH) levels, but symptom tracking is equally critical. Women who report persistent night sweats, vaginal dryness, or emotional lability may be strong candidates for early intervention. Moreover, evaluating family history and individual risk factors—such as osteoporosis or early heart disease—can offer additional guidance.
There is also an emerging awareness around age-specific considerations. The question “Can I take estrogen in my 30s?” is becoming increasingly common among women with premature ovarian insufficiency (POI) or surgical menopause. In such cases, early estrogen supplementation is not only safe but often recommended to protect long-term health. Female estrogen pills, patches, or creams can serve as targeted tools to address deficiencies that would otherwise go uncorrected for decades.

HRT Formulations: Choosing Between Estrogen Pills, Patches, and Bioidenticals
Once a woman decides to pursue HRT, the next step is selecting the appropriate formulation. The market offers various options, including estrogen pills, estrogen patches, creams, gels, vaginal rings, and bioidentical hormones. Each has its pros and cons, and the choice often hinges on lifestyle preferences, health history, and symptom profile.
Estrogen pills for women are among the most commonly prescribed forms and can be highly effective in alleviating symptoms such as hot flashes and night sweats. However, they pass through the liver, which may slightly elevate the risk of blood clots in certain individuals. For those seeking to avoid this, estrogen patch benefits are considerable. Patches deliver a consistent dose of hormones transdermally, bypassing hepatic metabolism and offering a safer profile for many women.
Bioidentical hormone therapies, often compounded to mimic the molecular structure of endogenous hormones, have grown in popularity due to their “natural” reputation. While some women swear by their effectiveness, it’s important to note that not all bioidenticals are FDA-approved, and quality control may vary. Regardless of the method chosen, the key is personalization. The best estrogen replacement is not a universal product—it is the one that works for a woman’s unique hormonal landscape.
When to Start Hormone Replacement Therapy: Navigating the Perimenopausal Years
Perimenopause presents a critical opportunity to consider when to start hormone replacement therapy. During this phase, hormone levels fluctuate unpredictably, causing symptoms that can last from a few months to several years. Many women mistakenly believe they must wait until menopause is officially confirmed before starting HRT, but that’s a myth that deserves to be dispelled.
Initiating hormone therapy during perimenopause can provide stability amidst hormonal chaos. This can be particularly helpful for women dealing with cycle irregularity, anxiety, or cognitive decline. Doctors often prescribe a combination of estrogen and cyclic progesterone during this time to help regulate periods while easing other systemic symptoms. Starting HRT during perimenopause may also provide neuroprotective benefits, reducing the long-term risk of dementia and preserving verbal memory.
The concern, “Is HRT safe for women during perimenopause?” is valid, but well-studied data supports its safety when appropriately prescribed. It is vital, however, to differentiate between over-the-counter hormone replacement therapy and clinically supervised regimens. The former often lacks the bioavailability and standardization needed to produce consistent results, making professional guidance non-negotiable.
Is Hormone Replacement Therapy Safe? Understanding the Risks and Benefits
The safety of HRT has been the subject of intense scrutiny, especially since the early 2000s when large-scale studies such as the Women’s Health Initiative (WHI) raised concerns about its long-term use. However, subsequent analyses revealed that many of those initial fears were overgeneralized. Today, we understand that the safety of hormone replacement therapy is strongly influenced by timing, formulation, and individual health history.
The benefits of HRT—when started within the optimal window—include reduced risk of osteoporosis, improved cognitive resilience, enhanced sexual health, and decreased vasomotor symptoms. Hormone replacement therapy side effects, when they do occur, are often mild and manageable. These may include breast tenderness, bloating, or slight mood swings, especially during the adjustment period.
Conversely, the risks—such as an increased chance of clotting or breast cancer—tend to manifest in older women or those with preexisting conditions. The question “Is hormone replacement therapy safe?” must therefore be answered on a case-by-case basis, not with blanket statements. With modern, low-dose formulations and individualized monitoring, HRT has become safer and more accessible than ever before.

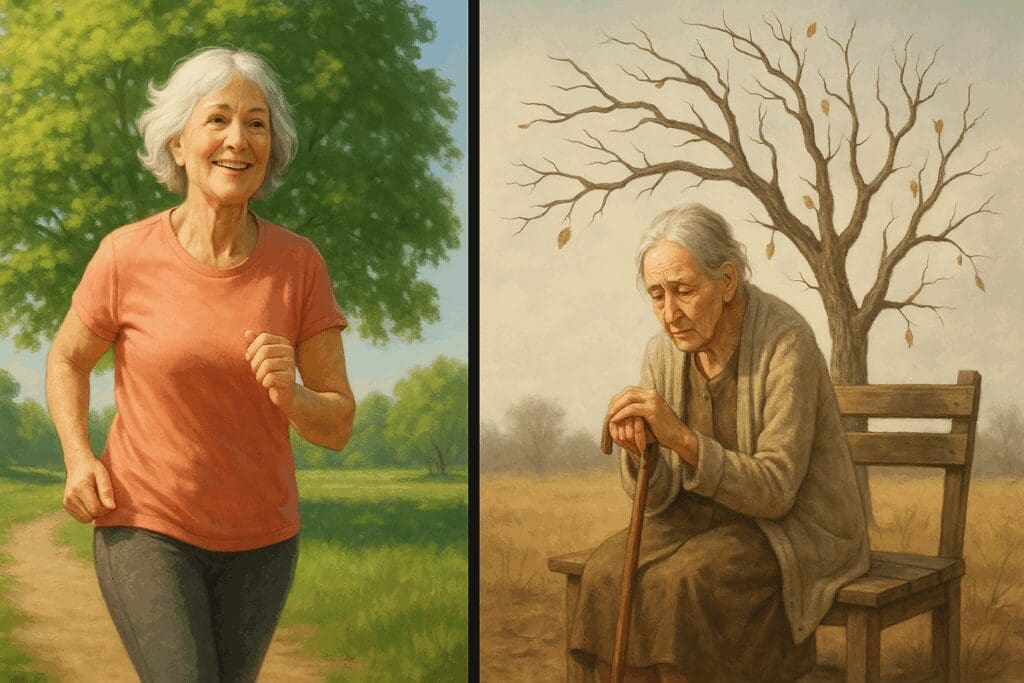
Hormone Replacement Before and After: Visualizing the Impact Over Time
To appreciate the transformative power of HRT, it helps to examine hormone replacement before and after initiation. Prior to therapy, many women report a decline in quality of life that affects their relationships, careers, and self-perception. They may struggle with fatigue, depression, and a diminished sense of self. These are not just inconveniences—they are barriers to thriving.
After starting HRT, the change can be profound. Many women describe a reawakening of vitality, clarity, and emotional equilibrium. They often sleep better, feel more mentally sharp, and reconnect with their bodies in a positive way. This “after” phase also brings practical benefits, such as reduced risk of fractures due to improved bone density and lower levels of inflammatory markers.
Of course, results vary, and no therapy is a panacea. However, for many women, hormone replacement offers a gateway to a more vibrant, energetic midlife. Documented improvements in lipid profiles, skin elasticity, and even muscle tone reinforce the idea that hormonal balance is not a luxury—it is a foundational pillar of health. Informed decisions about when to start hormone replacement therapy can make all the difference in this journey.
The Pros and Cons of Hormone Replacement Therapy: A Balanced Perspective
Exploring the pros and cons of hormone replacement therapy requires an honest, evidence-based approach that goes beyond sensational headlines or outdated assumptions. On the positive side, HRT can significantly alleviate the burdens of menopause. Women often experience dramatic relief from hot flashes, night sweats, vaginal dryness, and insomnia. These improvements in comfort and function can ripple outward, enhancing everything from mood to productivity to intimacy. Furthermore, clinical trials support HRT’s protective effects against osteoporosis, with data showing improved bone mineral density and reduced fracture rates. For many, these benefits alone justify consideration of therapy.
Yet, no medical intervention is without its drawbacks. HRT side effects may include nausea, breast tenderness, and breakthrough bleeding, especially during the early stages of use. Some women report headaches or mild bloating, although these symptoms typically resolve as the body adapts. More seriously, certain women—especially those who begin HRT later in life or have untreated hypertension—may face elevated risks for blood clots or cardiovascular complications. These risks, however, are significantly mitigated when HRT is initiated during the early postmenopausal years, reinforcing the importance of understanding when to start hormone replacement therapy.
Ultimately, the pros and cons of HRT are highly individualized. They depend on factors such as age, health status, genetic predispositions, and lifestyle choices. What remains clear is that with thoughtful timing, appropriate formulations, and professional oversight, the benefits often outweigh the risks for the majority of healthy, early postmenopausal women. This balanced viewpoint helps women make confident decisions based on scientific understanding rather than fear.

What Are the Signs That You Need Hormone Replacement Therapy?
Identifying what are the signs that you need hormone replacement therapy begins with a careful inventory of physical, emotional, and cognitive symptoms. One of the first indications is a persistent decline in quality of life. This may manifest as chronic fatigue, mood disturbances, or a loss of motivation. Many women describe feeling like “a different person” as estrogen levels wane—a phenomenon not to be dismissed as merely psychological. Hormones orchestrate a wide range of biological processes, and their depletion affects everything from neurotransmitter balance to metabolic efficiency.
Physical signs also play a crucial role. Vaginal dryness, painful intercourse, decreased libido, or recurrent urinary tract infections may signal estrogen deficiency. Likewise, sudden weight gain around the abdomen, thinning hair, and brittle nails may indicate broader hormonal imbalances. Sleep disruption, joint pain, and cognitive fog often worsen over time without hormonal support, leading many women to ask, “How do you know if you need HRT?” The answer often lies in a constellation of symptoms that point toward systemic decline rather than isolated issues.
For women experiencing early menopause or who have undergone hysterectomy or oophorectomy, the signs can be even more acute. In these cases, hormone replacement is not just optional—it can be essential for maintaining bone density, cardiovascular integrity, and neurological health. Listening to your body, tracking symptoms, and consulting a hormone-literate practitioner are all key steps in recognizing when intervention is appropriate.
When to Start Hormone Replacement Therapy: A Window of Opportunity for Optimal Health
The repeated question—when to start hormone replacement therapy—points to a deeper desire for proactive, preventative care. The ideal window, supported by numerous studies, is within ten years of menopause or before the age of 60. This window aligns with the body’s remaining capacity to respond favorably to estrogen and progesterone supplementation. Starting HRT during this time frame allows for a smoother hormonal transition, greater symptom relief, and a lowered risk of chronic disease.
However, women must also consider their own health histories when evaluating this timeline. For example, women with a personal or family history of breast cancer may need to explore non-hormonal options or use specialized formulations under strict medical supervision. Even within the recommended initiation window, the dosage and delivery method should be personalized. The goal is not merely to add hormones, but to restore a balanced endocrine environment in sync with the body’s needs.
Waiting too long to begin therapy can narrow your options. This is especially important when considering what are the risks of HRT after 70. Starting HRT at an advanced age—especially with underlying vascular disease—has been associated with higher risks for stroke and thrombosis. By contrast, timely intervention offers benefits that extend well beyond symptom relief, including neuroprotection and enhanced metabolic function. This is why medical professionals increasingly emphasize the concept of a therapeutic “window of opportunity” for hormone therapy.

Is HRT Safe for Women? Separating Myth from Modern Medical Consensus
The evolving consensus on HRT safety reflects decades of research, reassessment, and clinical experience. Early alarm about HRT, fueled by misinterpretation of the WHI study, has given way to a more refined understanding. Today, the question “Is HRT safe for women?” must be answered with clarity and context. For most healthy women who start therapy before age 60 or within ten years of menopause, HRT is not only safe—it can be highly beneficial.
Key factors influencing HRT safety include age, route of administration, and the presence of coexisting medical conditions. For instance, using a transdermal estrogen patch reduces clotting risks compared to oral pills. Low-dose regimens minimize exposure while still providing effective symptom control. Additionally, the use of micronized progesterone—considered the safest form—further reduces concerns around breast cancer and cardiovascular events.
Healthcare providers are increasingly comfortable prescribing HRT when it is warranted. Professional organizations such as the North American Menopause Society and the Endocrine Society have publicly supported the use of hormone therapy when tailored to individual needs. Their position underscores that the question is no longer “Is hormone replacement therapy safe?” but rather, “How can it be used most effectively and responsibly?”
OTC Hormone Replacement Therapy: Understanding the Limitations
Over-the-counter hormone replacement therapy is often marketed as a convenient, “natural” alternative to prescription treatments. Products like phytoestrogen creams, DHEA supplements, and herbal blends are readily available and promise relief from menopausal symptoms. However, these offerings present several challenges and should not be seen as substitutes for medically supervised HRT.
First and foremost, OTC formulations are not subject to the same regulatory scrutiny as prescription hormones. This means that potency, purity, and consistency can vary widely between brands—and even between batches. Inaccurate dosing may lead to subtherapeutic results or unintended side effects. Moreover, without proper testing or medical oversight, underlying conditions such as thyroid dysfunction or adrenal fatigue may go undiagnosed and untreated.
While some women do report mild symptom relief from over-the-counter products, these solutions often fail to address the root cause of hormonal decline. They may be useful as complementary therapies, but should not replace bioidentical or FDA-approved treatments when hormonal deficiency is significant. When deciding on an approach, it is always wise to seek expert guidance rather than rely solely on self-directed experimentation.
How to Take Estrogen Safely and Effectively
For women new to hormone therapy, the question of how to take estrogen is both practical and important. Estrogen can be administered in various ways, each with unique implications for absorption, metabolism, and risk. Oral pills are convenient but pass through the liver, which can slightly increase the risk of clotting or elevated triglycerides. For this reason, women with certain risk profiles may be better suited to non-oral methods.
Transdermal options, such as patches and gels, offer steady hormone delivery and bypass first-pass liver metabolism. These forms are often preferred for women with migraines, high blood pressure, or clotting disorders. Vaginal creams and rings, while limited in systemic absorption, are ideal for addressing localized symptoms such as dryness or urinary discomfort. The best estrogen replacement method depends on a woman’s specific needs, preferences, and risk factors.
Regular monitoring is also essential. Baseline labs, followed by periodic blood work, help track hormone levels and adjust dosing as needed. Ongoing assessment ensures that therapy remains both effective and safe. Whether using estrogen pills for women or other forms, the goal is always to achieve balance—not excess. A measured, thoughtful approach to how to take estrogen sets the foundation for long-term success.
Is Estrogen Replacement Therapy Safe? Dispelling Persistent Concerns
The question “Is estrogen replacement therapy safe?” often emerges from outdated fears and misinformation. When prescribed and monitored by qualified practitioners, estrogen therapy is safe for the vast majority of women entering menopause. The key is context: age, health status, and timing matter enormously. Starting therapy in a woman’s 50s yields markedly different outcomes than initiating it in her 70s.
Scientific literature supports the cardiovascular, skeletal, and cognitive benefits of estrogen when used appropriately. Data also suggest that estrogen alone—particularly in women without a uterus—carries a lower breast cancer risk than previously thought. Furthermore, the use of transdermal formulations and micronized progesterone has dramatically improved the safety profile of HRT overall.
Persistent concerns should be discussed openly with healthcare providers. Risk calculators and individualized assessments are invaluable tools for making informed decisions. No woman should feel forced to suffer through menopause out of fear or confusion. The modern landscape of HRT is one of personalized medicine, not one-size-fits-all prescriptions. In this context, estrogen replacement therapy is not just safe—it can be a critical pillar of preventive health.
What Are the Risks of HRT After 70?
For women over 70, hormone replacement therapy becomes a more complex decision. The body’s ability to metabolize hormones changes with age, and long-term vascular or metabolic issues may make late-life HRT less advisable. Clinical data suggest an increased risk of stroke, deep vein thrombosis, and gallbladder disease when therapy is initiated later in life, particularly after years of estrogen deficiency.
That said, not all risks are universal. Some women who have been on continuous HRT since their 50s may safely continue under supervision. The main concern is not ongoing use, but rather late initiation in previously untreated women. Starting HRT after 70 may be warranted in exceptional cases—such as severe osteoporosis or intractable vasomotor symptoms—but it demands heightened vigilance and risk-benefit evaluation.
This is where individualized care shines. Physicians must consider a woman’s full medical history, genetic profile, and symptom burden before initiating treatment. A cautious approach—perhaps using localized estrogen or ultra-low-dose systemic therapy—may offer benefits without undue risk. While HRT after 70 is not the norm, it is not categorically unsafe when used judiciously.
FAQ: Expert Insights on Hormone Replacement Therapy—Timing, Safety, and Strategies
1. When to Start Hormone Replacement Therapy to Support Mental and Cognitive Health?
The decision about when to start hormone replacement therapy (HRT) has implications beyond physical symptoms—it may also influence long-term brain health. Emerging studies suggest that initiating HRT during early perimenopause or soon after menopause may support memory, concentration, and mood regulation. This “critical window” hypothesis proposes that starting hormone replacement therapy when estrogen levels begin to decline may offer the most neurological protection. However, timing must be weighed against individual risk factors such as stroke, migraine history, or family predisposition to dementia. If you’re considering whether and when to start hormone replacement therapy for mental clarity or emotional balance, consult a clinician who can tailor recommendations based on your cognitive goals and neuroendocrine profile.
2. How Do You Know If You Need HRT for More Than Just Hot Flashes?
People often ask, “How do you know if you need HRT?”—but the answer goes beyond the presence of night sweats or vaginal dryness. Subtle signs like recurring UTIs, sudden joint stiffness, anxiety spikes, and even dry eyes can point to estrogen deficiency. If you’re asking yourself, “Do I need hormone replacement therapy?” consider how these symptoms affect your quality of life. A hormonal panel, pelvic ultrasound, and DEXA scan for bone density may uncover hidden risks that strengthen the case for starting HRT. Ultimately, your personal symptom burden, medical history, and goals—not just common menopausal markers—determine the answer to “do I need HRT.”
3. Is Hormone Replacement Therapy Safe for Women with Autoimmune or Inflammatory Conditions?
For those with autoimmune disorders like lupus or rheumatoid arthritis, the question “is hormone replacement therapy safe” demands a nuanced answer. While HRT can sometimes exacerbate systemic inflammation, newer formulations—especially transdermal options like estrogen patches—pose a lower risk. The estrogen patch benefits women with inflammatory conditions by bypassing the liver and reducing clotting risks. Still, treatment must be customized: low-dose strategies and bioidentical hormones may minimize flares while offering the benefits of HRT. If you’re navigating both menopause and autoimmune challenges, work with a rheumatologist and gynecologist collaboratively to determine if HRT is safe in your context.
4. Can I Take Estrogen in My 30s for Premature Ovarian Insufficiency?
Yes, you absolutely can—and often should. If you’re wondering, “Can I take estrogen in 30s?” due to early menopause, surgical removal of ovaries, or ovarian insufficiency, estrogen replacement therapy is typically recommended. Without it, you face higher risks of osteoporosis, cardiovascular issues, and cognitive decline. The best estrogen replacement in such cases mimics the body’s natural hormones and may include estrogen pills for women or patches depending on your metabolism and lifestyle. While OTC hormone replacement therapy options exist, medical-grade therapies ensure proper hormone levels, safety monitoring, and integration with fertility or bone health plans.
5. What Are the Pros and Cons of HRT for Women in Their Late 60s and 70s?
When evaluating the pros and cons of hormone replacement therapy in older age, it’s crucial to assess both symptom severity and long-term risk profiles. On the plus side, the benefits of HRT in this group may include better bone density, improved skin elasticity, and reduced urinary tract symptoms. However, what are the risks of HRT after 70? These may include elevated cardiovascular risks and higher chances of stroke, especially if HRT is started for the first time at this age. A thorough risk-benefit discussion with a physician is essential, particularly if you’re contemplating HRT for age-related issues rather than menopause symptom management.
6. How to Take Estrogen Safely for Best Results and Minimal Side Effects?
Understanding how to take estrogen effectively begins with choosing the right delivery method for your body’s needs. While estrogen pills are common, many find that patches or gels reduce liver strain and produce more stable mood and energy levels. To avoid common hormone replacement therapy side effects—such as breast tenderness, nausea, or bloating—it’s best to start with the lowest effective dose and monitor response regularly. Lifestyle factors, such as alcohol intake, fiber consumption, and body fat percentage, can also influence how your body processes estrogen. The best estrogen replacement is one that works in sync with your physiology, so dosage and timing should be adjusted over time.
7. Hormone Replacement Before and After: What to Expect Beyond Symptom Relief
The transformation seen in hormone replacement before and after is not just physical. Many women report improved interpersonal relationships, increased motivation, and regained confidence after initiating HRT. Beyond hot flash relief, female estrogen pills can support libido, mental sharpness, and even reduce social withdrawal caused by fatigue or irritability. Still, these benefits of HRT are accompanied by a need for realistic expectations—it may take weeks to months to feel full effects, and regular adjustments may be needed. Comparing hormone replacement before and after photos may be superficial; tracking mood, sleep, and energy changes tells a deeper story of success.
8. When to Start Hormone Replacement Therapy for Maximum Cardiovascular Protection?
Knowing when to start hormone replacement therapy may influence your future heart health more than you think. Evidence suggests initiating therapy within 10 years of menopause onset or before age 60 is associated with reduced risks of coronary artery disease. This is in contrast to initiating HRT later in life, when arterial plaques may already be established, increasing clotting risks. The pros and cons of hormone therapy in this context must be carefully balanced: while early HRT may be cardio-protective, starting late can pose significant complications. If you’re seeking the benefits of HRT for your heart, timing may be just as crucial as the choice of hormone.
9. Are OTC Hormone Replacement Therapy Options Worth Trying?
OTC hormone replacement therapy products, including herbal estrogen mimics and progesterone creams, appeal to many due to convenience and cost. However, these are not regulated like prescription treatments, making their efficacy and safety highly variable. While some may offer mild symptom relief, they lack the precision of medical hormone replacement therapy, especially in cases requiring tight hormonal control. If you’re evaluating OTC hormone replacement therapy options, consider them as complementary rather than primary solutions. Discuss any over-the-counter product use with your healthcare provider, particularly if you’re also on estrogen pills or patches, to avoid dosing conflicts or side effects.
10. Is HRT Safe for Women with a Family History of Breast Cancer?
For women with a familial predisposition to breast cancer, the question “is HRT safe for women” is especially sensitive. The answer depends heavily on the type of HRT (e.g., estrogen-only vs. combined estrogen-progestin), route of administration, and duration. Estrogen patch benefits in this case include a more favorable safety profile compared to oral pills, especially in hysterectomized women. That said, even the best estrogen replacement therapy must be personalized and monitored closely. Genetic testing, like BRCA screening, and consultations with oncology-informed gynecologists are essential when deciding whether hormone replacement therapy is safe in this scenario.
Conclusion: Embracing Empowered Choices About Hormone Health
The journey through menopause is deeply personal, and decisions around hormone therapy must reflect a woman’s unique physiology, history, and aspirations for the future. Understanding when to start hormone replacement therapy is a cornerstone of that journey, offering a powerful opportunity to preserve vitality, protect against chronic disease, and reclaim a sense of wholeness during midlife and beyond. As we’ve explored, initiating HRT within the optimal window—typically before age 60 or within ten years of menopause—can significantly enhance safety and efficacy.
For those wondering, “Do I need HRT?” or “What are the signs that you need hormone replacement therapy?” the answers lie in both science and self-awareness. From the benefits of HRT to the evolving safety profile of modern therapies, today’s landscape empowers women with more options and better outcomes than ever before. Whether using estrogen pills, patches, or bioidentical alternatives, hormone therapy can offer profound relief and renewal.
Navigating the pros and cons of hormone replacement therapy requires not only medical insight but also self-trust and curiosity. It is a decision best made with guidance, but never out of fear. By asking the right questions, understanding the critical timing of intervention, and working with knowledgeable practitioners, women can make informed choices that support lifelong hormonal balance and holistic well-being.
Further Reading:
All about hormone replacement therapy (HRT)



