Vaginal dryness during period may seem paradoxical to many, especially given the general association of menstruation with increased moisture and discharge. However, for countless individuals, dryness in the vaginal area is a recurring and uncomfortable reality during their menstrual cycle. This seemingly contradictory symptom can cause both physical discomfort and emotional distress, affecting not only daily life but also intimacy, hygiene, and overall well-being. Understanding the surprising causes behind this dryness, as well as how to find relief, is essential for anyone navigating the complex landscape of hormonal changes and vaginal health.
While it may be tempting to chalk up any dryness to environmental factors or personal hygiene habits, the reality is far more nuanced. Vaginal dryness is often a multifactorial issue influenced by hormonal fluctuations, lifestyle choices, medications, and underlying medical conditions. This is particularly true during menstruation, when hormone levels are in flux and estrogen—the hormone largely responsible for maintaining vaginal moisture—is at its lowest. The result can be an environment that feels tight, dry, and even painful, leading many to question, “Why am I dry down there all of a sudden?”
This article will take a deep dive into the medical, hormonal, and lifestyle-related causes of vaginal dryness during period, along with evidence-based and expert-recommended strategies for alleviating this distressing condition. From exploring the impact of birth control and breastfeeding to identifying the best vulva moisturizer or the most effective external vaginal moisturizer, our goal is to equip you with the knowledge and tools to better understand, manage, and treat this condition. Whether you’re experiencing a dry vagina before period or facing dryness throughout your cycle, the following sections will provide comprehensive insights grounded in both science and lived experience.
You may also like: Debilitating Cramps Don’t Have to Ruin Your Month: Ovira Is the Off Switch for Period Pain

Hormonal Shifts and the Hidden Role of Estrogen in Vaginal Dryness During Period
Estrogen plays a pivotal role in maintaining the health of the vaginal tissues, ensuring they remain thick, elastic, and well-lubricated. During the menstrual cycle, estrogen levels are not constant; they dip significantly during menstruation and then rise again as the body prepares for ovulation. It is precisely during this dip that many individuals experience vaginal dryness during period. The loss of estrogen not only leads to a decrease in vaginal lubrication but can also cause the vaginal walls to become thinner and more susceptible to irritation.
This hormonal shift doesn’t just impact lubrication—it also affects blood flow to the vaginal area. Reduced blood circulation means less nutrient delivery to the vaginal tissues, exacerbating the sensation of dryness, tightness, and discomfort. In some cases, this can even lead to small tears or microabrasions during physical activity or intercourse, which may increase the risk of infection or inflammation.
It’s worth noting that this cycle of estrogen fluctuation is a normal part of reproductive physiology. However, for some individuals, particularly those who are more sensitive to hormonal changes, these shifts can feel pronounced and debilitating. Women on hormonal birth control or hormone-modulating medications may find these patterns altered or amplified. In such cases, dryness may persist not only during menstruation but throughout the cycle, raising concerns about how to increase vaginal wetness and maintain comfort across hormonal phases.
Understanding the hormonal roots of dryness opens the door to more targeted treatments. Whether through localized estrogen therapy in cases of extreme vaginal atrophy or through lifestyle adaptations that support hormonal balance, relief is possible. While not everyone will require medical intervention, being aware of this biological rhythm is the first step in reclaiming comfort and confidence.
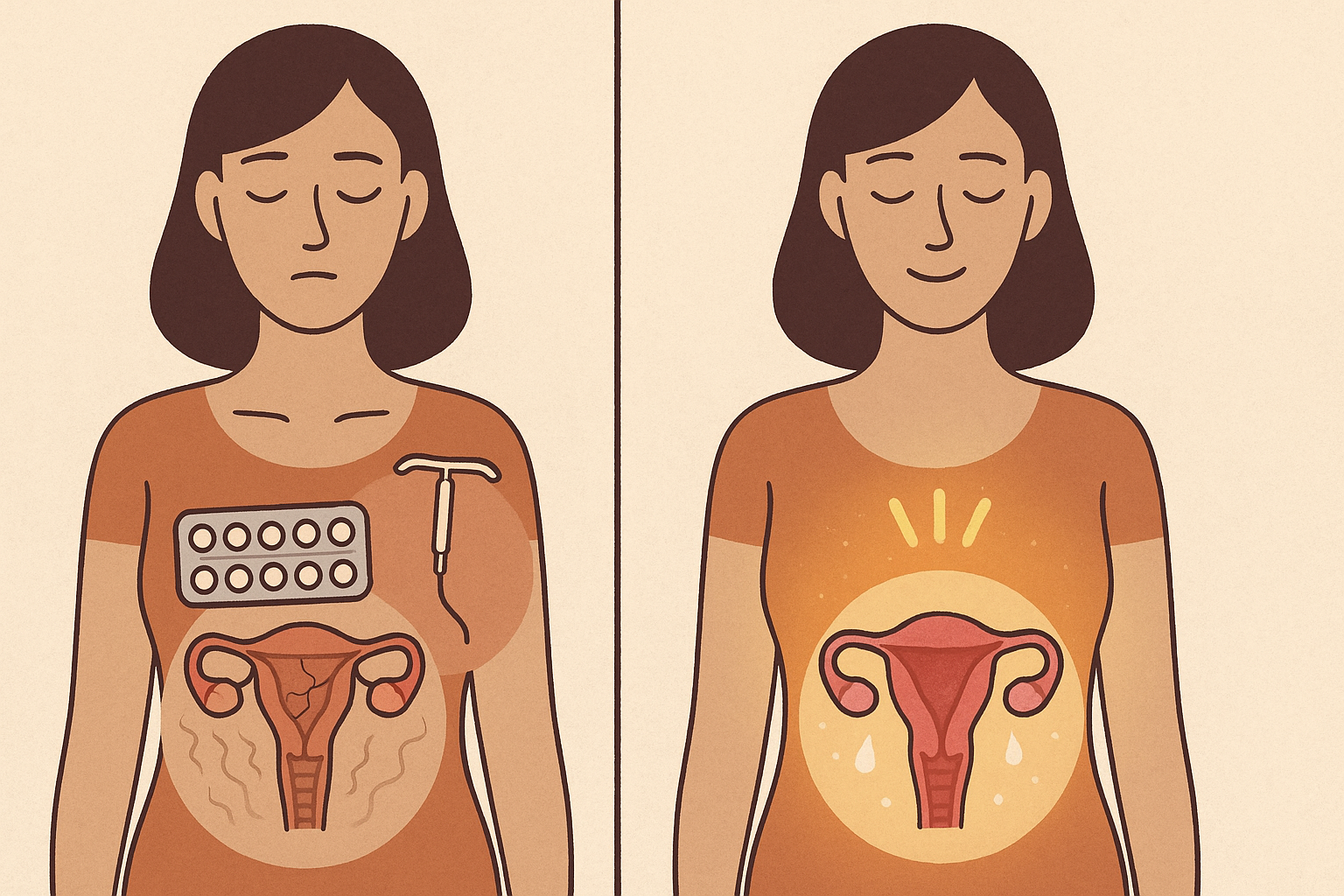
The Connection Between Birth Control and Vaginal Dryness During Period
One of the more surprising and often overlooked contributors to vaginal dryness during period is hormonal birth control. While designed to regulate menstruation, prevent pregnancy, and manage hormonal conditions, these medications often contain synthetic hormones that suppress the body’s natural estrogen production. The result is a lower baseline of estrogen throughout the cycle, which can lead to a persistent state of dryness—even during menstruation when moisture would normally be expected.
This effect can be particularly pronounced in individuals using progestin-only birth control methods, such as the mini-pill, hormonal IUDs, or certain contraceptive implants. Progestin can thin the endometrial lining and suppress cervical fluid production, leading to an overall reduction in vaginal lubrication. The irony is that while birth control is often prescribed to alleviate heavy or painful periods, it can inadvertently introduce a different type of discomfort in the form of vaginal dryness.
For those wondering how to fix dryness from birth control, the solution may lie in both internal and external strategies. Switching to a combined hormonal method that includes estrogen or transitioning to a non-hormonal contraceptive may be options worth exploring with a healthcare provider. Additionally, incorporating the best vaginal moisturizer into one’s daily routine can provide immediate symptomatic relief.
Moreover, understanding that birth control-related dryness is not a failure of the body but rather a side effect of synthetic hormonal modulation can shift the narrative from frustration to empowerment. With a clearer understanding of how these medications influence vaginal tissue, individuals can make more informed decisions about their reproductive and sexual health.
Breastfeeding and Postpartum Changes That Trigger Vaginal Dryness
Another commonly underrecognized factor contributing to vaginal dryness during period—especially among postpartum individuals—is breastfeeding. Lactation induces a unique hormonal state characterized by elevated prolactin levels and suppressed estrogen. This hormonal landscape is biologically designed to support milk production, but it often comes at the expense of vaginal lubrication and elasticity.
This breastfeeding dryness can feel particularly harsh when combined with the hormonal upheaval of menstruation resuming after childbirth. Some individuals may experience dryness so severe that it mimics symptoms of vaginal atrophy, such as itching, burning, or discomfort during intercourse. These symptoms are not only physically painful but can also undermine intimacy and emotional closeness, especially during a time of significant life transition.
Finding relief during this phase involves a careful balance of self-care, hydration, and appropriate product use. The best vulva moisturizer and external vaginal moisturizer options are typically non-hormonal and formulated with hyaluronic acid, aloe vera, or vitamin E to provide both immediate and long-term hydration. These products are safe to use while breastfeeding and can significantly improve comfort without interfering with milk production.
Additionally, understanding that this dryness is a normal, albeit uncomfortable, part of the postpartum experience can reduce shame and anxiety. Just as the body needs time to recover physically, the reproductive system needs time to reestablish hormonal equilibrium. With the right support and information, breastfeeding individuals can navigate this stage with confidence and clarity.
What Causes Vaginal Dryness During Period Beyond Hormones?
Although hormonal fluctuations are a significant factor, they are far from the only cause of vaginal dryness during period. Environmental factors, hygiene products, medications, and underlying medical conditions can all contribute to a decrease in natural lubrication. For instance, the frequent use of scented tampons, menstrual pads, or cleansing wipes can disrupt the delicate pH balance of the vaginal area, leading to irritation and moisture loss.
Certain medications—particularly antihistamines, antidepressants, and chemotherapy drugs—are also known to reduce vaginal secretions. These side effects may intensify during menstruation when the body is already more sensitive to changes. Additionally, autoimmune disorders such as Sjögren’s syndrome or thyroid imbalances can further complicate the issue, presenting symptoms that mimic or worsen vaginal dryness.
Another overlooked contributor is stress. Chronic stress impacts the hypothalamic-pituitary-adrenal (HPA) axis, which in turn influences estrogen and cortisol levels. The resulting hormonal imbalance can reduce blood flow and lubrication in the genital area, making the vaginal tissues more susceptible to dryness and discomfort. This raises the question of how to stay lubricated during sex when stress and menstruation collide.
Lifestyle choices such as excessive exercise, smoking, or alcohol use can also dehydrate the body and diminish vaginal moisture. Each of these elements—though seemingly unrelated—plays a role in the broader ecosystem of vaginal health. Understanding these surprising contributors empowers individuals to look beyond the obvious and adopt a more holistic approach to vaginal dryness treatment.
Recognizing Vaginal Atrophy and When to Seek Help
For some individuals, vaginal dryness during period may be an early indicator of vaginal atrophy—a condition commonly associated with menopause but increasingly recognized in younger populations. Also known as atrophic vaginitis, this condition is characterized by thinning, drying, and inflammation of the vaginal walls due to a significant drop in estrogen levels. Symptoms can include persistent dryness, itching, burning, and painful intercourse, particularly in the days leading up to or during menstruation.
Recognizing vaginal atrophy symptoms early is crucial for initiating timely and effective treatment. While hormonal replacement therapy (HRT) is often used to treat moderate to severe cases, non-hormonal treatments such as vaginal moisturizers and lubricants can be effective for milder symptoms. When exploring how to treat atrophic vaginitis, it’s important to choose products that are free from fragrances and irritants and are specifically formulated for the sensitive vaginal environment.
For individuals concerned about the progression of symptoms or the impact on quality of life, consulting a gynecologist or pelvic health specialist can provide clarity. These professionals can evaluate hormone levels, conduct a pelvic exam, and recommend personalized treatment plans that may include prescription estrogen creams, vaginal dilators, or specialized physical therapy.
In many cases, what starts as occasional dryness may evolve into a chronic issue if not addressed. Early recognition and intervention not only provide physical relief but also preserve long-term sexual and reproductive health. Understanding how to treat vaginal atrophy and recognizing when dryness signals a deeper issue are essential skills for anyone navigating menstrual or menopausal changes.
Navigating Vaginal Dryness Before and After Your Period
It’s important to recognize that vaginal dryness is not confined solely to the menstruation window; many individuals experience dryness before and after their period as well. This cyclical variation is directly linked to the hormonal phases of the menstrual cycle. During the luteal phase—the time between ovulation and menstruation—progesterone levels are higher and estrogen begins to decline. This hormonal environment can lead to dryness before period, sometimes accompanied by feelings of tightness or a mild burning sensation.
Similarly, in the days following menstruation, vaginal tissue may still be recovering from the hormonal and physical demands of the period. This is especially true if a person has been using products that alter the pH or has been under added stress. This period of vulnerability may result in increased sensitivity, making a dry vagina before period feel even more uncomfortable in the post-menstrual phase.
To counter these changes, many gynecologists recommend maintaining a consistent self-care routine that includes the use of gentle, pH-balanced cleansers, daily application of the best vaginal moisturizer, and avoiding overly drying hygiene products. Understanding the natural rise and fall of vaginal lubrication throughout the month allows individuals to anticipate dryness and respond proactively rather than reactively. For those struggling with dryness across multiple phases of the cycle, it may be helpful to chart symptoms alongside the menstrual calendar to detect patterns and explore personalized treatment strategies.

How to Treat Vaginal Dryness During Period: Practical and Medical Solutions
Once the causes are identified, the next step is addressing how to treat vaginal dryness in a way that is both effective and sustainable. Treatment options range from simple lifestyle changes to over-the-counter products and prescription therapies. For many, the first line of defense involves selecting the best vaginal moisturizer that provides long-lasting hydration without disrupting the natural flora of the vaginal area. These moisturizers are designed for daily use and work differently from lubricants, which are used to reduce friction during intercourse.
Lubricants can be a powerful tool for immediate relief, especially when dryness interferes with intimacy. Choosing the right lubricant for dry vagina symptoms involves avoiding alcohol-based or fragranced products and opting instead for water-based or silicone-based formulas that offer both comfort and safety. For those asking how to stay lubricated during sex, using a high-quality, dermatologist-recommended lubricant is an excellent starting point.
In cases where dryness is severe or persistent, particularly when accompanied by signs of atrophy, medical interventions may be necessary. Vaginal estrogen therapy—available in creams, rings, or tablets—can restore moisture and elasticity by replenishing local estrogen levels. This treatment is especially effective for postmenopausal individuals or those with medically induced hormonal suppression. However, even in younger patients, doctors may prescribe low-dose estrogen if dryness significantly impacts quality of life. These strategies, combined with behavioral changes such as staying hydrated, reducing stress, and maintaining sexual activity (which promotes blood flow), create a multi-pronged approach to treating vaginal dryness during period effectively and safely.
External and Internal Support: Best Vulva and Vaginal Moisturizers to Consider
Choosing the right moisturizing products can make a significant difference in managing and preventing vaginal dryness, particularly during menstruation. The best vulva moisturizer is one that is specifically formulated for external use, free of harsh chemicals and irritants, and capable of restoring hydration without altering the natural microbial balance. These products typically include soothing ingredients like aloe vera, vitamin E, and calendula, which reduce irritation while reinforcing the skin barrier.
Meanwhile, internal vaginal moisturizers are inserted directly into the vaginal canal and offer extended hydration by mimicking the body’s natural secretions. These products are often used every few days rather than daily and can be especially helpful for individuals experiencing dryness during multiple phases of their cycle. For example, someone struggling with dryness before period and during menstruation may find relief through a combination of internal and external moisturizing routines.
For those concerned about allergies or sensitivity, hypoallergenic and fragrance-free options are essential. Product labels should be scrutinized for terms like “gynecologist-tested,” “non-hormonal,” and “pH-balanced” to ensure compatibility with the unique needs of the vaginal ecosystem. Some individuals may even find relief using prescription-strength moisturizers or estrogen-based products under medical supervision. Regardless of the product chosen, consistency is key. Applying moisturizer regularly, even outside of acute episodes of dryness, can help maintain tissue integrity and prevent future flare-ups.
What Does Vaginal Dryness Feel Like? Understanding Sensations and Subtle Clues
Many individuals are uncertain whether what they’re experiencing is truly vaginal dryness or simply part of normal hormonal fluctuations. To answer the question “what does vaginal dryness feel like,” it’s helpful to describe both the physical sensations and the contextual triggers that often accompany this symptom. Common feelings include tightness, burning, itching, or a sensation of friction during movement. In some cases, dryness can also cause microtears, leading to mild bleeding or a sharp, stinging discomfort.
Emotionally, dryness can create anxiety or insecurity, especially around intimacy. Someone who previously enjoyed pain-free intercourse may suddenly wonder, “Why am I tight and dry?” This shift can be disorienting and distressing, particularly when it arises unexpectedly. Dryness can also affect day-to-day activities, from walking to exercising, and may even lead to discomfort when wearing certain fabrics like synthetic underwear or tight-fitting clothing.
The key to identifying true vaginal dryness lies in noticing these subtle but persistent changes in sensation, particularly if they coincide with specific times in the menstrual cycle. Being able to articulate the symptoms clearly to a healthcare provider can lead to faster diagnosis and more effective treatment. Whether it’s a dryness before period, during menstruation, or in between, paying close attention to how the body feels can be an invaluable step toward finding lasting relief.

How to Increase Vaginal Wetness and Support Long-Term Hydration
Once the root causes of dryness are identified and acute symptoms are managed, the next question becomes how to increase vaginal wetness consistently over time. Fortunately, there are several strategies—both medical and holistic—that support long-term vaginal hydration and tissue health. A diet rich in omega-3 fatty acids, phytoestrogens, and adequate hydration can enhance mucosal membrane function throughout the body, including the vaginal lining. Foods like flaxseeds, salmon, walnuts, and soy products may promote better lubrication by supporting hormone production and tissue elasticity.
In terms of lifestyle, regular sexual activity—including masturbation—has been shown to increase blood flow and stimulate natural lubrication. For individuals who are sexually active, communication with a partner about dryness and the use of a suitable lubricant can transform discomfort into an opportunity for intimacy and connection. For those less sexually active, vaginal dilators or pelvic floor exercises can offer similar benefits by increasing circulation and preventing atrophy.
Some may also benefit from supplements that support vaginal health. Products containing DHEA (dehydroepiandrosterone), vitamin E, or sea buckthorn oil are increasingly being studied for their role in enhancing vaginal moisture. While these should never replace medical advice, they offer promising adjunctive support for those looking to learn how to increase vaginal fluid through safe, natural means. Ultimately, consistency and a comprehensive approach are the keys to staying lubricated and comfortable across all stages of the menstrual cycle and beyond.
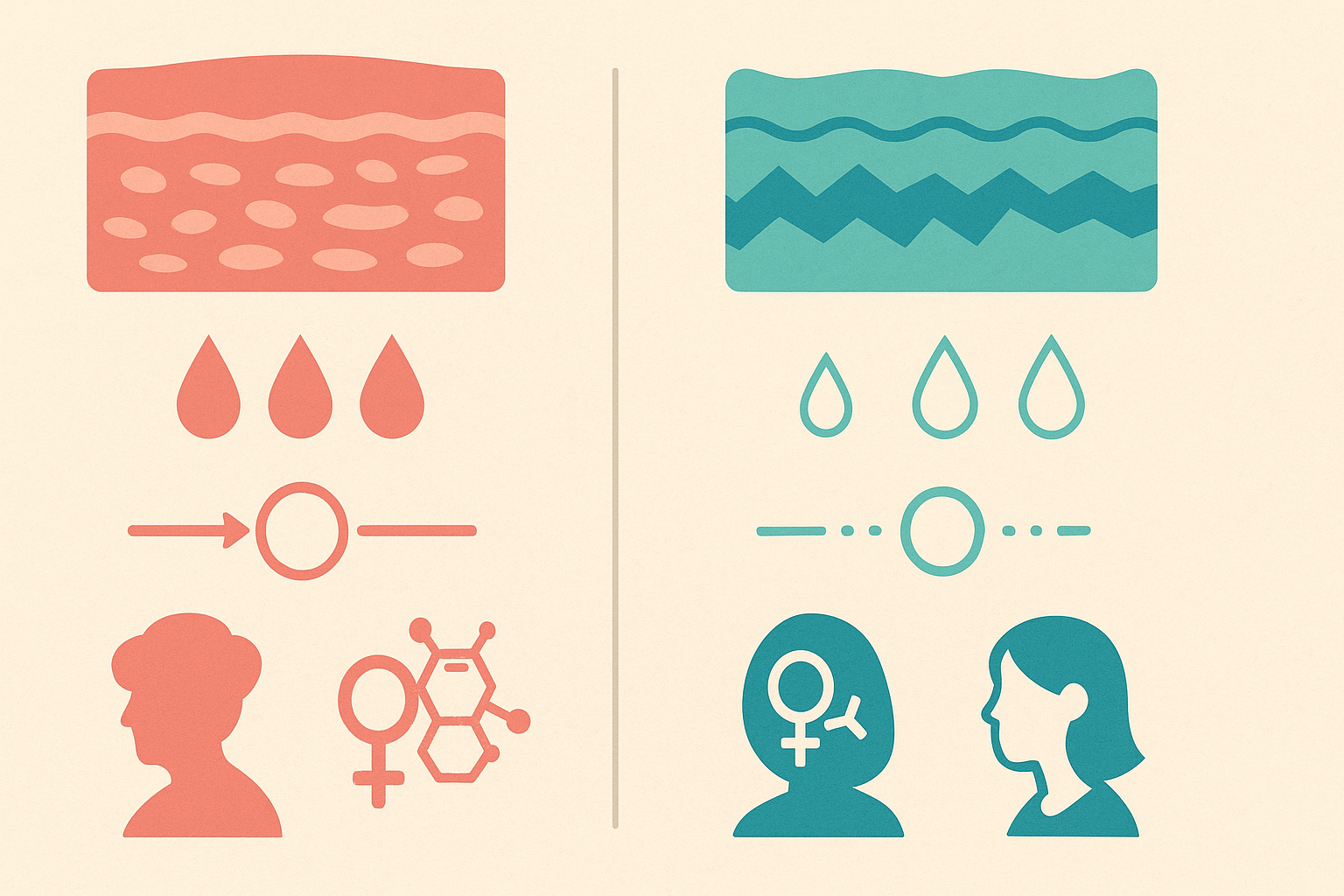
Atrophic Vaginitis vs. Temporary Vaginal Dryness: Knowing the Difference
Differentiating between temporary vaginal dryness and atrophic vaginitis can be challenging but is essential for proper treatment. While both conditions may present with similar symptoms—such as discomfort, tightness, and irritation—the underlying causes and treatment approaches are quite distinct. Temporary dryness often correlates with hormonal dips during menstruation or specific external triggers, while atrophic vaginitis involves long-term structural changes in the vaginal tissue due to chronically low estrogen levels.
Atrophic vaginitis is more common during menopause but can also occur in younger women due to medical conditions, breastfeeding, or long-term contraceptive use. Symptoms often include persistent burning, itching, painful intercourse, and increased susceptibility to urinary tract infections. Individuals wondering how to treat vaginal atrophy may require targeted estrogen therapy or advanced non-hormonal treatments to reverse the tissue thinning and restore hydration.
In contrast, treating occasional vaginal dryness during period may not require hormonal treatment but rather supportive care such as the use of moisturizers, lubricants, and stress management techniques. Recognizing the chronicity and severity of symptoms is critical to determining which path to pursue. Whether the dryness is a temporary response to menstrual shifts or part of a larger hormonal imbalance, proper diagnosis ensures that the chosen treatment is not only effective but also sustainable in the long term.
Why Is My Vagina So Dry and Itchy? When to Be Concerned
While occasional dryness is often harmless, there are times when dryness is accompanied by other symptoms that warrant further investigation. Itchiness, for example, is not always a typical symptom of menstrual dryness and may indicate the presence of a yeast infection, bacterial vaginosis, or allergic reaction. For individuals asking “why is my vagina so dry and itchy,” it’s important to look at the full clinical picture, including any changes in discharge, odor, or color.
Sometimes the culprit may be as simple as an irritating laundry detergent, douching, or tight synthetic clothing that doesn’t allow the area to breathe. Other times, the root issue could be more serious—such as lichen sclerosus, contact dermatitis, or even early indicators of autoimmune disorders. In these instances, the best course of action is to consult with a gynecologist who can perform the necessary tests and recommend an appropriate course of treatment.
Dryness paired with itching can significantly disrupt daily life and interfere with both sleep and intimacy. Fortunately, many of these underlying issues are easily treatable with antifungals, antibiotics, or topical corticosteroids. In the meantime, using a high-quality vulva moisturizer and avoiding known irritants can provide temporary relief and prevent further aggravation.
How to Stay Lubricated During Intercourse When Dealing with Vaginal Dryness
For many people, one of the most distressing aspects of vaginal dryness is its impact on sexual intimacy. Pain during intercourse, known medically as dyspareunia, can strain relationships and erode self-confidence. The question of how to stay lubricated during intercourse is both a physical and emotional one, requiring a multifaceted approach that includes preparation, communication, and product use.
First and foremost, using a lubricant for dry vagina symptoms is non-negotiable when dealing with dryness. The best lubricants are those that are pH-balanced, free from irritants, and tailored to long-lasting comfort. Silicone-based lubricants tend to offer more durability, while water-based options are easier to clean and compatible with condoms and toys. Application should be generous and may even include reapplication mid-encounter to ensure continued comfort.
Beyond lubrication, communication with one’s partner is vital. Talking openly about needs, discomforts, and preferences can transform what might be an awkward or painful experience into one of connection and mutual care. Taking extra time for foreplay, adjusting sexual positions, and incorporating sensual touch can also improve the experience by stimulating natural lubrication and relaxing the pelvic muscles.
For those still struggling, working with a sexual health counselor or pelvic floor therapist can yield surprising benefits. These professionals can help identify tension, trauma, or physical barriers to comfort and develop personalized strategies for improvement. By addressing both the mechanical and emotional dimensions of vaginal dryness during period and beyond, couples can reclaim pleasure and intimacy in ways that feel safe and empowering.
Why Am I Dry Down There All of a Sudden? When Sudden Changes Signal Something More
One of the most jarring experiences is the sudden onset of vaginal dryness in someone who has never struggled with it before. This abrupt shift often leads individuals to ask, “Why am I dry down there all of a sudden?” The answer may lie in recent changes to medication, stress levels, sexual activity, or hormonal fluctuations. Even minor lifestyle shifts—such as starting a new skincare regimen, changing detergents, or enduring a stressful life event—can trigger vaginal sensitivity and dehydration.
Medical causes should also be considered. A sudden drop in estrogen, whether due to perimenopause, significant weight loss, or illness, can precipitate dryness. Thyroid dysfunctions, particularly hypothyroidism, are another common but overlooked cause. In rare cases, dryness may also be an early symptom of autoimmune disease, making it essential to track and report any additional symptoms to a healthcare provider.
If the dryness persists for more than a few weeks or is accompanied by pain, itching, or discharge, it’s important to seek medical advice. Early detection can prevent more serious complications and lead to faster, more effective treatment. By paying attention to one’s body and being proactive about changes, individuals can navigate sudden vaginal dryness with confidence and clarity.
Frequently Asked Questions About Vaginal Dryness During Period: Insights and Solutions Beyond the Basics
1. Why might vaginal dryness during period feel more uncomfortable than at other times?
Vaginal dryness during period can feel especially distressing because menstruation temporarily alters the balance of pH, estrogen levels, and mucosal hydration in the vaginal environment. This combination can heighten sensitivity and reduce the protective barrier typically provided by vaginal secretions. Furthermore, tampon use—common during menstruation—can absorb not only menstrual blood but also natural lubrication, aggravating the sensation of dryness. Some women also experience dryness-related itching or a tight, raw feeling due to frequent cleansing or the use of scented hygiene products, which can strip away moisture. This discomfort can be significantly reduced by switching to unscented, organic period products and using an external vaginal moisturizer specifically designed for menstrual use.
2. How is vaginal dryness before period different from vaginal dryness during period?
Vaginal dryness before period, also called dryness before period, is usually linked to the natural dip in estrogen levels that occurs during the luteal phase of the menstrual cycle. This dip results in decreased cervical fluid production and a reduction in vaginal blood flow, leading to a tighter, less lubricated sensation. In contrast, vaginal dryness during period may involve more complex triggers, including inflammation from shedding of the uterine lining, mechanical irritation from hygiene products, or even concurrent hormonal conditions like PCOS. Both types of dryness can co-occur, making diagnosis and treatment more nuanced. If you’re unsure of your pattern, consider tracking your symptoms across two or three cycles to identify whether you’re experiencing dry vagina before period, during menstruation, or both.
3. What does vaginal dryness feel like when it’s hormonally driven versus when it’s caused by lifestyle factors?
Hormone-related vaginal dryness—such as that experienced during perimenopause, breastfeeding, or menstruation—often feels like persistent internal tightness, stinging, or a burning sensation that isn’t relieved by hydration or hygiene changes. In contrast, dryness from lifestyle factors (like excessive washing or certain fabrics) is often more localized to the outer vulvar area and may be accompanied by visible skin irritation or flakiness. Many women describe hormonally driven dryness as feeling as though their vagina is “shrinking” or “closing up,” which reflects the atrophic changes associated with decreased estrogen. If you’re wondering why is my vagina dry or why am I tight and dry, tracking both hormonal fluctuations and environmental exposures can help pinpoint the underlying cause. This distinction is key for choosing the correct treatment—whether that’s a vulva moisturizer, lifestyle changes, or hormonal therapy.
4. Can birth control pills contribute to dryness, and how to fix dryness from birth control effectively?
Yes, hormonal contraceptives can significantly impact natural lubrication, especially those containing high levels of progestin. This hormone suppresses ovulation and, in turn, reduces the body’s production of estrogen—a key player in vaginal lubrication. If you’re experiencing symptoms and asking how to fix dryness from birth control, consider switching to a formulation with lower progestin or adding a topical vaginal estrogen under medical supervision. Non-hormonal remedies like the best vaginal moisturizer or best vulva moisturizer can also provide daily hydration and restore comfort. It’s important to avoid self-medicating with over-the-counter estrogen creams without consulting a healthcare provider, as improper use may cause hormonal imbalances or exacerbate existing symptoms.
5. How does breastfeeding dryness differ from vaginal dryness during period in terms of treatment needs?
Breastfeeding dryness stems primarily from suppressed estrogen production during lactation, a natural consequence of elevated prolactin levels. While the sensation may feel similar to vaginal dryness during period, the treatment approach must consider the needs of a postpartum body. Breastfeeding mothers may prefer non-hormonal interventions, such as using an external vaginal moisturizer or water-based lubricant for dry vigina concerns. It’s also worth noting that breastfeeding dryness often affects both the vagina and vulva more diffusely, which may call for combination therapy using both internal and external hydration products. If the discomfort is interfering with intimacy or daily activities, ask your OB-GYN about compatible treatments like hyaluronic acid gels or postpartum-safe vaginal moisturizers.
6. What’s the link between vaginal atrophy and persistent vaginal dryness—even in menstruating women?
While vaginal atrophy is often associated with menopause, it can occur in younger menstruating women with hormonal imbalances, especially those with eating disorders, extreme stress, or chronic illness. If you’re wondering how to treat vaginal atrophy or how to treat atrophic vaginitis, it’s essential to first confirm the diagnosis with a vaginal pH test and physical examination. Atrophic changes cause the vaginal walls to thin, dry, and lose elasticity, which makes lubrication alone insufficient. In these cases, vaginal atrophy treatment may require estrogen therapy alongside a high-quality lubricant for dry vigina use. Emerging treatments like laser therapy or DHEA vaginal inserts are also showing promise for long-term relief without systemic side effects.
7. How to increase vaginal wetness naturally and stay lubricated during intercourse without synthetic hormones?
If you’re seeking how to increase vaginal fluid or how to stay lubricated during intercourse without using hormonal treatments, there are several proven methods. Diet plays a role—omega-3 fatty acids, flaxseeds, and soy can help balance hormones and enhance mucosal hydration. Staying hydrated and managing stress through mindfulness or adaptogens like ashwagandha may also enhance arousal-based lubrication. Additionally, pelvic floor physical therapy can improve blood flow and tissue responsiveness, which helps you stay lubricated during sex. Using plant-based lubricants and daily application of the best vaginal moisturizer can also mimic natural fluids and promote lasting comfort.
8. Why am I dry down there all of a sudden if I’ve never experienced vaginal dryness before?
Sudden onset vaginal dryness can be caused by a range of unexpected triggers: new medications (like antihistamines, antidepressants, or diuretics), abrupt hormonal shifts due to illness or intense exercise, or even undiagnosed thyroid issues. Ask yourself why is my vagina dry or why is my vigina so dry and itchy—these may be signals of an underlying systemic change. Infections like yeast or bacterial vaginosis can also cause inflammation that mimics dryness symptoms even when discharge is present. An external vaginal moisturizer may relieve symptoms short-term, but it’s important to investigate deeper if the dryness doesn’t resolve in a week or two. A full hormonal panel, thyroid test, and review of your medication list can uncover root causes.
9. How does vaginal dryness after birth evolve over time, and what are long-term treatment strategies?
Vaginal dryness after birth is often overlooked in postpartum care, yet it affects up to 60% of women in the months following delivery. Initially, it’s caused by reduced estrogen, but other contributors include vaginal trauma, stitches, and breastfeeding-related hormonal shifts. While many women expect the issue to resolve on its own, how to treat vaginal dryness after birth often requires a dedicated regimen: gentle hydration with the best vulva moisturizer, consistent use of an external vaginal moisturizer, and—for persistent cases—discussion of estrogen therapy. Importantly, returning to penetrative intimacy before addressing dryness may worsen symptoms and delay healing. Long-term treatment should also consider pelvic floor health and emotional well-being, especially for women who experience fear or pain related to intercourse postpartum.
10. Understanding Vaginal Dryness During Period: How to Treat and Prevent Future Flare-Ups
If you’re navigating vaginal dryness during period repeatedly, you may need to think beyond short-term fixes. Long-term strategies include regulating estrogen levels through stress management, ensuring micronutrient intake (especially vitamin D and B-complex), and avoiding exposure to parabens or sulfates in hygiene products. For acute care, the best vaginal moisturizer can offer multi-day hydration, and pairing it with a vulva moisturizer ensures both internal and external relief. Be proactive in choosing period products: silicone cups and organic pads are less drying than traditional tampons or synthetic liners. And if you’re continually asking how to treat vaginal dryness without lasting success, a gynecologist may recommend hormonal mapping or personalized estrogen therapy to ensure your cycle is functioning optimally.
Conclusion: Reclaiming Comfort and Confidence by Understanding Vaginal Dryness During Period
Vaginal dryness during period is a complex, multifaceted issue that affects a wide range of individuals, often in silence and confusion. While it may seem counterintuitive to feel dry during a time associated with menstrual flow, the truth lies in the body’s intricate hormonal dance. From fluctuations in estrogen and the effects of hormonal birth control to the challenges of breastfeeding and postpartum recovery, there are numerous pathways through which dryness can take hold.
Yet, with knowledge comes empowerment. By understanding what causes vaginal dryness, recognizing early signs of vaginal atrophy, and identifying effective solutions—from the best vulva moisturizer to how to increase vaginal wetness through diet, products, and sexual wellness—individuals can reclaim both physical comfort and emotional well-being. Whether dealing with temporary discomfort or managing a chronic condition, it is possible to restore balance, pleasure, and confidence through informed choices and compassionate care.
As we continue to destigmatize conversations about vaginal health, let this be an invitation to explore one’s body with curiosity and kindness. Whether you’re seeking answers to why your vagina feels dry and itchy, how to treat atrophic vaginitis, or how to stay lubricated during intercourse, remember that you’re not alone—and that real, lasting relief is within reach.
Further Reading:
Vaginal dryness: Symptoms, causes, remedies