As women transition into the perimenopausal stage, the body undergoes profound hormonal shifts that can significantly affect mood, metabolism, sleep, and energy levels. These changes make it more important than ever to adopt a targeted perimenopause nutrition plan designed to support hormonal balance and sustained vitality. The right diet not only helps ease symptoms like hot flashes, irritability, and fatigue, but also nourishes the body to support long-term health. In this comprehensive guide, we’ll explore the critical role of nutrition during perimenopause and provide a scientifically grounded approach to optimizing diet for energy, balance, and resilience.
You may also like: The Essential Guide to Balanced Nutrition: Building Healthier Habits That Last

Understanding Perimenopause: The Hormonal Landscape
Perimenopause refers to the transitional phase leading up to menopause, often beginning in a woman’s 40s but sometimes starting as early as the mid-30s. During this time, levels of estrogen, progesterone, and even testosterone fluctuate unpredictably. These hormonal shifts can cause a cascade of symptoms—ranging from night sweats and weight gain to mood swings and memory fog. Understanding the biological framework of perimenopause is essential to crafting a nutrition plan that supports the body’s evolving needs.
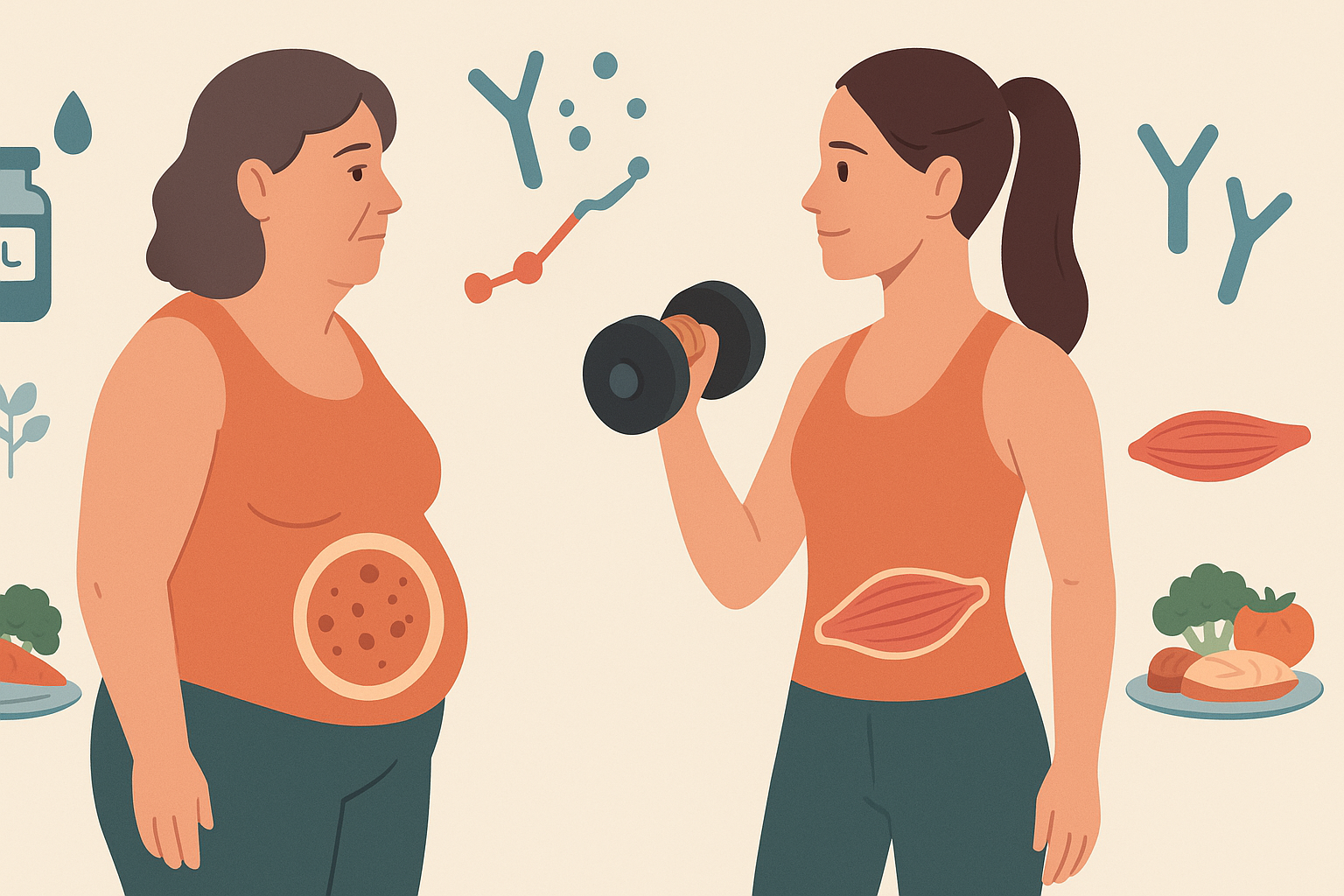
Estrogen, a hormone central to reproductive function, also influences bone density, cardiovascular health, and even neurotransmitter activity. As estrogen production slows, women often experience a decrease in muscle mass and a redistribution of body fat, especially around the abdomen. Progesterone, which plays a calming role in the nervous system, also diminishes, contributing to anxiety and sleep disturbances. A well-crafted perimenopause diet must be tailored to help buffer these hormonal fluctuations through strategic nutrient support.
Why Diet Matters More Than Ever in Perimenopause
During perimenopause, the body becomes more sensitive to dietary patterns. Insulin resistance may increase, appetite-regulating hormones like leptin and ghrelin can become dysregulated, and inflammatory markers may rise. These shifts make a compelling case for adopting the best diet for perimenopause—one that emphasizes nutrient density, hormonal harmony, and blood sugar stability.
A poor diet can exacerbate perimenopausal symptoms by promoting inflammation, blood sugar spikes, and nutrient deficiencies. On the other hand, foods for perimenopause that are rich in phytoestrogens, fiber, healthy fats, and adaptogenic compounds can help modulate estrogen levels, soothe the nervous system, and support adrenal function. This isn’t about restriction; it’s about strategic nourishment that aligns with the body’s changing rhythms.

Crafting the Perimenopause Nutrition Plan: Core Principles
Developing an effective perimenopause nutrition plan begins with a focus on nutrient synergy rather than calorie counting. Each meal should be composed with hormonal health in mind, prioritizing key macronutrients and micronutrients that support metabolic stability, endocrine function, and cellular repair.
First and foremost, every meal should balance protein, healthy fats, and complex carbohydrates. Protein is essential for preserving lean muscle mass, especially as estrogen declines. Healthy fats—such as those found in avocados, nuts, seeds, and fatty fish—support hormone synthesis and combat inflammation. Complex carbohydrates from vegetables, legumes, and whole grains help stabilize blood glucose, reduce cravings, and feed gut microbes that produce mood-regulating neurotransmitters.
Fiber intake is also paramount. A diet rich in soluble and insoluble fiber supports digestion, helps remove excess estrogen through the bowels, and feeds beneficial gut bacteria. Flaxseeds, chia seeds, lentils, and leafy greens are excellent choices. Including probiotic and prebiotic foods can further enhance the gut’s role in estrogen metabolism.
Finally, hydration and micronutrient adequacy are key. Electrolyte-rich beverages like coconut water or herbal teas can support adrenal health, while minerals like magnesium, zinc, and calcium help maintain sleep quality, mood balance, and bone integrity.
The Best Foods for Perimenopause: What to Eat and Why
Identifying the best foods for perimenopause requires understanding how individual nutrients affect hormonal pathways. Phytoestrogens—plant compounds that mimic estrogen—can help buffer declining estrogen levels. Foods like fermented soy (tempeh, miso), flaxseeds, sesame seeds, and chickpeas are excellent sources. Regular consumption may ease hot flashes and promote hormonal equilibrium.
Omega-3 fatty acids, found in salmon, sardines, walnuts, and flax oil, play a central role in reducing systemic inflammation. These fats also support brain function, cardiovascular health, and hormonal fluidity. Including fatty fish at least twice per week can make a measurable difference in symptoms like joint pain, brain fog, and mood swings.
Magnesium-rich foods like spinach, pumpkin seeds, dark chocolate, and almonds are particularly beneficial for managing perimenopause fatigue, sleep disturbances, and muscle cramps. Magnesium supports over 300 enzymatic processes, many of which are tied to stress modulation and energy production.
Cruciferous vegetables—such as broccoli, kale, Brussels sprouts, and cauliflower—contain indole-3-carbinol and sulforaphane, compounds that support liver detoxification of excess estrogen. Their role in hormone metabolism makes them a staple in any healthy diet for perimenopause.
Lastly, don’t overlook vitamin D and calcium-rich foods. As bone density declines, ensuring adequate intake of these nutrients is essential. Wild salmon, sardines with bones, fortified plant milks, and leafy greens can provide a solid foundation for skeletal health.

Perimenopause Nutrition Plan: Daily Meal Structure for Energy and Balance
A well-structured perimenopause nutrition plan follows predictable rhythms that align with the body’s natural circadian and hormonal cycles. Starting the day with a protein-rich breakfast stabilizes blood sugar and cortisol, the body’s wake-up hormone. Options like a spinach and mushroom omelet with avocado, or Greek yogurt with chia seeds and berries, can jump-start metabolism while minimizing energy crashes.
Lunch should emphasize fiber and complex carbs to sustain energy through the afternoon. Think lentil soup with leafy greens, or quinoa salad with roasted vegetables and tahini dressing. Including a source of fermented food—like sauerkraut or kimchi—adds digestive support and helps modulate immune responses.
Afternoon snacks should support adrenal function and stave off blood sugar dips. A handful of walnuts with an apple, or hummus with cucumber slices, delivers a combination of healthy fats, fiber, and phytoestrogens. Avoid sugary or carb-heavy snacks that trigger insulin spikes and leave you feeling sluggish.
Dinner is an ideal time to emphasize anti-inflammatory foods and calming nutrients like magnesium and tryptophan. Baked salmon with steamed broccoli and sweet potatoes offers a powerhouse of brain-supporting fats, detoxification aids, and complex carbs that ease tension and aid sleep.
Maintaining consistent meal timing also supports hormonal regulation. Intermittent fasting can be helpful for some, but it must be adapted thoughtfully in perimenopause. Women experiencing adrenal fatigue or high stress should avoid overly restrictive windows, as fasting can exacerbate symptoms.
The Best Diet for Menopausal Women vs. Perimenopausal Needs
While the best diet for menopausal women shares many principles with a perimenopause meal plan, the timing and focus of nutrients may differ slightly. Perimenopause involves active hormonal fluctuation, so the emphasis lies in balancing estrogen and supporting detox pathways. Once menopause arrives and estrogen levels stabilize at a lower baseline, maintaining bone health and metabolic rate becomes even more critical.
That said, perimenopause is the gateway to menopause, making early adoption of supportive nutrition habits an investment in long-term well-being. Diets like the Mediterranean, DASH, and anti-inflammatory protocols align well with both stages. These plans emphasize plant-based diversity, healthy fats, and lean proteins while minimizing processed foods and sugars.
The Mediterranean diet, in particular, has been shown to reduce perimenopausal symptoms, improve cardiovascular health, and stabilize weight. Its rich inclusion of olive oil, legumes, whole grains, herbs, and seafood makes it both delicious and hormonally nourishing. For women seeking the best diet for menopausal women that also supports the transition phase, Mediterranean-inspired eating offers a timeless blueprint.

Foods to Avoid During Perimenopause: Triggers and Trouble-Makers
Just as certain foods support hormonal harmony, others can trigger or worsen perimenopausal symptoms. Highly processed foods, refined sugars, and trans fats are major culprits. These items promote inflammation, spike blood sugar, and disrupt gut microbiota, creating a cascade of negative effects on mood, sleep, and metabolism.
Caffeine and alcohol can also exacerbate symptoms like night sweats, anxiety, and sleep disruption. While moderate consumption may be tolerable for some, women struggling with insomnia or heart palpitations may benefit from reducing or eliminating these substances. Swapping coffee for matcha or herbal teas like chamomile or lemon balm can offer a gentler energy lift without overstimulating the nervous system.
Excess sodium and low-fiber diets can contribute to bloating, constipation, and water retention—issues that many perimenopausal women face. Prioritizing hydration, potassium-rich produce, and whole plant foods can counterbalance these effects.
Lastly, be mindful of xenoestrogens—chemical compounds found in certain plastic containers, non-organic animal products, and cosmetics. These endocrine disruptors can mimic estrogen in the body and worsen hormonal imbalances. Choosing organic produce, grass-fed meats, and toxin-free packaging reduces the burden on your hormonal system.
Perimenopause Fatigue and the Role of a Supportive Diet
Fatigue during perimenopause can feel relentless, often tied to poor sleep, hormonal crashes, and nutrient deficiencies. Addressing this through diet means focusing on blood sugar regulation, mitochondrial support, and adrenal resilience. A perimenopause diet that includes adaptogenic herbs, slow-burning carbohydrates, and B-vitamin-rich foods can provide steady energy throughout the day.
Adaptogens like ashwagandha, rhodiola, and holy basil can be incorporated through teas, powders, or supplements. These herbs help buffer stress, reduce cortisol overproduction, and enhance energy regulation. Combined with nutrient-dense foods like eggs, leafy greens, quinoa, and legumes, they form the foundation of a menopause fatigue diet that nourishes without overstimulating.
Stabilizing blood sugar is essential. Meals and snacks should never be skipped, and protein should anchor every plate. Spikes and crashes in glucose levels can lead to brain fog, irritability, and the afternoon slump that so many women describe. By building meals that avoid refined grains and sugar, energy becomes more sustainable and predictable.
Magnesium and iron deficiencies are also common culprits. Including foods like pumpkin seeds, lentils, and dark leafy greens ensures the body has the building blocks to make ATP—the energy currency of cells. Pairing iron-rich foods with vitamin C sources like bell peppers or citrus fruits enhances absorption.
What to Eat for Menopause Support: Bridging the Transition
As perimenopause progresses toward menopause, dietary strategies should evolve to reflect the body’s changing needs. Bone support becomes increasingly important as estrogen’s protective effects wane. Calcium-rich foods like tahini, sardines, and collard greens, paired with vitamin D from sunlight or fortified foods, help maintain skeletal strength.
Heart health also moves to the forefront. Estrogen plays a protective role in cholesterol metabolism, and its decline can increase cardiovascular risk. Diets high in soluble fiber, plant sterols, and omega-3s offer a natural buffer. Oats, apples, flaxseeds, and walnuts are all top choices.
Digestive changes may also emerge, with slowed motility and shifts in gut flora. Eating fermented foods, increasing fiber, and staying well-hydrated can help regulate elimination and reduce bloating. The perimenopause nutrition plan thus naturally transitions into a menopause eating plan by maintaining the same foundational principles while shifting emphasis toward longevity and prevention.
Personalizing the Perimenopause Diet Plan: One Size Doesn’t Fit All
Though general dietary principles can guide most women, personalizing a perimenopause diet plan based on symptoms, genetics, lifestyle, and pre-existing conditions is the gold standard. For instance, women with thyroid issues may need to focus on selenium and iodine-rich foods. Those with PCOS or insulin resistance should adopt lower-glycemic approaches, possibly incorporating elements of the ketogenic or paleo diets tailored for hormone balance.
Food sensitivities should also be evaluated. Gluten, dairy, and soy can be inflammatory triggers for some women, while acting as beneficial phytoestrogen sources for others. Working with a nutritionist or integrative practitioner can help identify personal triggers and customize a meal plan accordingly.
Tracking symptoms and food intake can also be illuminating. Keeping a journal to log meals, energy levels, mood, and sleep patterns may reveal patterns and correlations that support smarter dietary choices. Adjusting intake based on cycle patterns, stress levels, and seasonal changes is also a form of intuitive, adaptive nutrition.
The Perimenopause Nutrition Plan in Action: A Week of Balanced Meals
To bring the perimenopause nutrition plan to life, it helps to see how these principles translate into daily practice. A sample week of meals not only provides inspiration but also demonstrates how the best foods for perimenopause can be integrated effortlessly into a delicious, nourishing routine. While individual preferences, intolerances, and lifestyle demands vary, the following menu offers a versatile and nutrient-dense foundation.
A Monday might begin with a warm bowl of steel-cut oats cooked in almond milk, topped with ground flaxseeds, blueberries, and a sprinkle of cinnamon. This breakfast provides phytoestrogens, fiber, antioxidants, and blood sugar stabilization. Lunch could include a lentil and quinoa salad with arugula, chopped cucumbers, cherry tomatoes, and a lemon-olive oil vinaigrette. This midday meal balances plant protein, anti-inflammatory fats, and gut-supportive greens. For dinner, a fillet of baked salmon with roasted Brussels sprouts and a small baked sweet potato ensures a generous dose of omega-3s, sulfur compounds for detox, and slow-burning carbohydrates to support sleep.
Throughout the week, variety is key. Incorporating tempeh stir-fries with bok choy, wild rice bowls with edamame and tahini, and hearty vegetable soups with beans and whole grains prevents palate fatigue while delivering an array of micronutrients. Snacks like Greek yogurt with pumpkin seeds, a banana with almond butter, or even a hard-boiled egg with sea salt can maintain satiety and energy between meals.
Hydration should not be overlooked. In addition to water, herbal teas like nettle (rich in minerals), chamomile (calming), and peppermint (digestive support) offer therapeutic benefits. Limiting caffeinated beverages to early in the day and choosing non-stimulating alternatives in the evening supports cortisol balance and restful sleep.

Emotional Wellness and Nutrition: Food’s Role in Mood and Resilience
Perimenopause brings not only physical changes but emotional ones as well. Mood swings, irritability, anxiety, and even depressive symptoms can become more pronounced due to hormonal imbalances and neurotransmitter fluctuations. Fortunately, diet plays a meaningful role in regulating brain chemistry and enhancing emotional resilience.
Tryptophan, an amino acid found in turkey, eggs, and pumpkin seeds, serves as a precursor to serotonin—a key neurotransmitter involved in mood stabilization. Pairing tryptophan-rich foods with complex carbs (such as sweet potatoes or brown rice) helps enhance serotonin synthesis. Omega-3 fatty acids also contribute to mood regulation and have been studied extensively for their antidepressant properties. A diet low in omega-3s may contribute to increased irritability and brain fog, while consistent intake can reduce the frequency and intensity of mood swings.
B vitamins, especially B6, B9 (folate), and B12, are essential for the synthesis of neurotransmitters like dopamine and serotonin. These vitamins can be found in leafy greens, legumes, eggs, and organ meats. Women following plant-based diets may need to supplement with B12, as it is found predominantly in animal products.
Magnesium, often referred to as nature’s chill pill, also supports emotional balance. A healthy diet for perimenopause that includes magnesium-rich foods can reduce anxiety, ease PMS-like symptoms, and improve sleep quality. Avocados, dark chocolate, and legumes all contribute significantly to daily magnesium intake.
Finally, the gut-brain connection must not be ignored. A disrupted microbiome can influence mood via the gut-brain axis. Including probiotic foods like kefir, kimchi, and yogurt, along with prebiotic fibers from garlic, onions, and bananas, supports a healthier emotional baseline.
Hormonal Weight Gain and Metabolism: Rethinking Calories in Perimenopause
Weight gain during perimenopause is a common and frustrating experience for many women. Even those who have maintained the same lifestyle for decades may find themselves gaining weight, particularly around the midsection. While part of this shift is hormonal, diet and metabolic adaptation play equally critical roles.
Estrogen influences insulin sensitivity and fat distribution. As levels drop, the body becomes less efficient at managing blood glucose and more likely to store fat, particularly visceral fat. This not only affects appearance but also increases the risk of metabolic syndrome, type 2 diabetes, and cardiovascular disease.
The solution is not drastic caloric restriction, which can worsen metabolic decline and trigger muscle loss. Instead, the best diet for perimenopause emphasizes metabolic flexibility—teaching the body to use both carbohydrates and fats efficiently. This can be achieved by combining resistance training with a perimenopause meal plan that balances macronutrients, includes ample protein, and avoids blood sugar spikes.
Eating enough protein is essential for maintaining muscle mass and thermogenesis. Consuming 20–30 grams of protein per meal—found in foods like eggs, poultry, fish, lentils, and Greek yogurt—helps curb appetite and supports fat loss. In addition, spacing protein throughout the day rather than consuming it in one large meal enhances its effectiveness.
Meal timing also plays a role. Eating earlier in the day and avoiding late-night snacking aligns with circadian rhythms and can improve insulin sensitivity. This is especially useful for women experiencing night sweats, poor sleep, or sugar cravings in the evening.
Beyond Food: Lifestyle Practices That Complement the Perimenopause Nutrition Plan
While food is foundational, other lifestyle factors significantly influence how well a perimenopause nutrition plan performs. Sleep, stress, movement, and environmental exposures all interact with hormonal systems. Addressing these holistically amplifies the benefits of a well-designed diet.
Quality sleep is essential for hormonal repair and glucose regulation. Inadequate sleep increases cortisol, drives sugar cravings, and undermines weight management efforts. Creating a calming evening ritual, minimizing blue light exposure, and using sleep-promoting nutrients like magnesium and glycine can enhance sleep quality.
Stress management is equally vital. Chronic stress elevates cortisol, which interferes with sex hormone production and promotes belly fat storage. Daily practices such as breathwork, yoga, journaling, and nature walks help reduce the physiological load of stress. Paired with foods good for menopause, these habits form a powerful toolkit for hormonal harmony.
Movement should be viewed through the lens of nourishment rather than punishment. Resistance training, in particular, helps preserve bone density and lean muscle mass while improving insulin sensitivity. Weight-bearing exercises like walking, hiking, and dancing also support skeletal strength and cardiovascular health.
Minimizing exposure to endocrine disruptors from plastics, synthetic fragrances, and non-organic animal products further reduces hormonal interference. Choosing natural cleaning products, storing food in glass containers, and reading labels on skincare and cosmetics can make a measurable difference in hormone function.
Perimenopause Diet and Nutrition for Bone and Heart Health
Two critical health concerns during and after perimenopause are osteoporosis and heart disease. Estrogen plays a protective role in both domains, and its decline necessitates proactive dietary strategies to preserve bone integrity and cardiovascular resilience.
For bone health, calcium and vitamin D are central, but they do not act alone. Magnesium, vitamin K2, and boron also support calcium absorption and bone remodeling. Foods like sardines (with bones), tofu, leafy greens, almonds, and fermented dairy contribute a full spectrum of bone-building nutrients. Including strength training and weight-bearing activity amplifies these dietary efforts.
For heart health, fiber, antioxidants, and healthy fats are crucial. A menopause eating plan should include oats, barley, lentils, olive oil, avocado, and fatty fish to lower LDL cholesterol and reduce arterial inflammation. Polyphenol-rich foods like berries, pomegranate, and dark chocolate provide additional vascular support.
Regular intake of potassium-rich foods—bananas, sweet potatoes, and beans—helps manage blood pressure and electrolyte balance. Reducing added sugar and refined carbohydrates can also stabilize triglyceride levels and prevent endothelial dysfunction.
Empowering Women Through Education: What to Eat to Help Menopause
One of the most empowering tools for navigating perimenopause is knowledge. When women understand what to eat to help menopause and how to tailor nutrition to their unique physiology, they reclaim agency over their bodies. Education dismantles fear and replaces it with confidence, curiosity, and self-compassion.
Understanding the value of micronutrients, recognizing the effect of meal timing, and tuning into the body’s responses to different foods all strengthen a woman’s intuition and biological literacy. This isn’t about strict rules or one-size-fits-all regimens—it’s about fostering a dynamic, responsive relationship with nourishment.
For healthcare providers, educators, and coaches, promoting perimenopause nutrition as a central part of care encourages preventive strategies over reactive interventions. It invites collaboration, experimentation, and long-term commitment to vitality.
FAQ: Advanced Insights on Building a Sustainable Perimenopause Nutrition Plan
1. Why does a perimenopause nutrition plan need to evolve over time?
A successful perimenopause nutrition plan must be dynamic because hormone fluctuations don’t occur in a straight line. As estrogen and progesterone shift unpredictably, so do energy needs, insulin sensitivity, and inflammation levels. Early perimenopause may demand more focus on regulating blood sugar and supporting adrenal health, while late perimenopause often requires strategies to combat bloating, joint pain, and sleep disruption. Tracking symptoms in relation to food can help personalize adjustments. Regular check-ins with a registered dietitian can ensure your plan evolves with your body’s needs, making it more effective and sustainable long term.
2. What role does gut health play in the best diet for perimenopause?
Gut health is often overlooked in perimenopausal diet planning, but it significantly influences hormone regulation, mood, and metabolism. Estrogen is partially processed through the gut via the estrobolome, a community of gut bacteria that helps metabolize and excrete excess hormones. Dysbiosis can disrupt this process, potentially leading to estrogen dominance symptoms like irritability and heavy bleeding. Including prebiotic foods like leeks, artichokes, and oats along with probiotic-rich options such as kefir or kimchi can optimize digestion. A gut-supportive approach enhances the best diet for perimenopause by reducing systemic inflammation and supporting emotional well-being.
3. How can your perimenopause nutrition plan support better sleep?
Sleep issues are common during perimenopause due to fluctuating hormones, particularly falling progesterone. A perimenopause nutrition plan tailored to sleep should prioritize magnesium-rich foods (like pumpkin seeds, spinach, and quinoa) to relax the nervous system and regulate melatonin production. Limiting sugar and alcohol in the evening helps stabilize blood sugar and reduce nighttime cortisol spikes. Protein timing is also important—consuming tryptophan-rich foods such as turkey or cottage cheese with complex carbs may promote deeper sleep. Fine-tuning food intake to align with circadian rhythms can be a game-changer for sleep quality.
4. What foods help minimize inflammation and support joint health during perimenopause?
Inflammation can intensify perimenopausal symptoms, including joint pain and brain fog. Anti-inflammatory omega-3s found in sardines, walnuts, and flaxseeds are foundational to a healthy diet for perimenopause. Curcumin (from turmeric), anthocyanins (from berries), and gingerol (from ginger) have clinically supported anti-inflammatory effects and can be easily added to meals. Bone broth provides collagen and glycine, which support connective tissue and gut health. Choosing these foods for perimenopause offers functional benefits far beyond basic nutrition.
5. Can timing meals and snacks improve the effectiveness of a perimenopause diet plan?
Absolutely. Meal timing can regulate cortisol, insulin, and hunger hormones, which are all destabilized during perimenopause. A perimenopause diet plan that emphasizes a protein-rich breakfast within 60 minutes of waking may reduce cortisol spikes and mid-morning fatigue. Avoiding long fasting periods or skipping meals can prevent reactive hypoglycemia, a common issue as estrogen levels drop. Strategic snack timing—such as a light, protein-rich snack around 3 p.m.—can also curb cravings and prevent evening overeating. When to eat matters just as much as what to eat during perimenopause.
6. How does emotional eating change during this phase, and how can your diet support resilience?
Emotional eating often increases in perimenopause due to stress, poor sleep, and estrogen-related serotonin changes. A healthy diet for perimenopause should include mood-stabilizing nutrients like B-vitamins (in leafy greens), zinc (in seeds and seafood), and omega-3s (in fatty fish). Consistently nourishing your body reduces the biochemical drivers behind anxiety-induced snacking. Moreover, mindful eating practices—like checking in with hunger cues and setting mealtime rituals—can reduce impulsive behaviors. Incorporating foods good for menopause also supports dopamine balance, making it easier to resist processed foods and sugar.
7. What are some of the best overlooked micronutrients in a menopause eating plan?
While calcium and vitamin D are well-known, others like choline, selenium, and boron are often underappreciated in a menopause eating plan. Choline, found in eggs and liver, supports cognitive function and fat metabolism. Selenium, present in Brazil nuts, is vital for thyroid health—a common challenge during perimenopause. Boron enhances the body’s ability to use estrogen and vitamin D efficiently. These micronutrients subtly yet significantly elevate the quality of a perimenopause meal plan by addressing root causes of fatigue and metabolic slowdown.
8. How can you maintain muscle mass through nutrition during hormonal changes?
Estrogen helps preserve muscle mass, so its decline can lead to accelerated muscle loss, known as sarcopenia. Including 25–30 grams of protein per meal from a variety of sources like lentils, eggs, tempeh, and lean meats can counteract this loss. Leucine-rich foods (such as whey protein and poultry) are particularly effective at stimulating muscle protein synthesis. This is essential to any best diet for menopausal women seeking to maintain strength and metabolic flexibility. When paired with resistance training, a protein-conscious perimenopause nutrition approach can protect long-term physical independence.
9. What strategies help combat fatigue through a menopause fatigue diet?
Fatigue during perimenopause isn’t just about lack of sleep—it’s about mitochondrial function, thyroid support, and nutrient absorption. A menopause fatigue diet rich in B-complex vitamins, iron, and adaptogenic herbs like ashwagandha or rhodiola can restore cellular energy. Swapping refined carbs for fiber-rich alternatives like sweet potatoes and lentils stabilizes glucose levels and prevents energy crashes. Hydration, often ignored, plays a vital role; even mild dehydration amplifies exhaustion. These strategies extend beyond conventional wisdom about what to eat to help menopause fatigue and provide real-life energy solutions.
10. What future trends are emerging in healthy eating for perimenopause?
Personalized nutrition is the frontier of healthy eating for perimenopause. Advances in microbiome testing, continuous glucose monitoring, and epigenetic screening are reshaping how we define the best diets for menopause. Tech-enabled insights allow women to see how specific foods affect their blood sugar, stress levels, or sleep in real time. Plant-based phytoestrogens are being explored more deeply for their adaptive benefits. As research grows, a perimenopause diet and nutrition protocol will likely be tailored not just to the stage of life, but to the individual’s unique genetic and metabolic fingerprint—making perimenopause wellness more targeted and transformative than ever.
Reflecting on the Power of Nutrition in Perimenopause and Beyond
Perimenopause is a profound biological and emotional transition, one that reshapes a woman’s body, identity, and future. Yet, with the right tools and information, it becomes a time of reconnection and empowerment rather than confusion and depletion. A thoughtful, evidence-based perimenopause nutrition plan offers not only symptom relief but also a deeper relationship with the body’s innate intelligence.
By emphasizing whole, nutrient-rich foods, balancing blood sugar, supporting hormone detoxification, and addressing emotional well-being, women can navigate perimenopause with strength and clarity. The best diet for perimenopause isn’t a rigid program—it’s a flexible, supportive framework that evolves with the woman herself.
As estrogen wanes, the wisdom of nourishment rises. Food becomes more than sustenance; it becomes medicine, mood stabilizer, hormone ally, and energy source. What to eat during perimenopause and what to eat for menopause are not simply academic questions—they are deeply personal, powerful choices that shape a woman’s health trajectory for years to come.
In honoring this transition with compassion, science, and self-awareness, we unlock the true potential of food as a lifelong partner in well-being. Whether you’re seeking the best foods for menopause or a tailored perimenopause meal plan, remember that your body already holds the answers—you’re simply learning to listen more deeply, and to nourish more wisely.
Further Reading:
Menopause Diet: What To Eat To Help Manage Symptoms
Menopause Diet: How What You Eat Affects Your Symptoms



