Navigating the hormonal turbulence of midlife can be both confusing and overwhelming. For many women entering perimenopause—the transitional phase leading up to menopause—one particularly uncomfortable symptom that frequently emerges is the hot flash. While these sudden waves of heat and sweating are widely associated with hormone fluctuations, there’s a growing body of evidence that suggests lifestyle factors also play a significant role in their intensity and frequency. One such factor, often overlooked, is alcohol consumption. Understanding the connection between perimenopause and alcohol is essential for those seeking to manage hot flashes effectively and reclaim a sense of bodily control and emotional balance during this pivotal time.
While a glass of wine or cocktail might offer temporary relaxation or social enjoyment, alcohol has complex effects on the female body, particularly one already undergoing hormonal shifts. Many women report increased hot flashes after drinking, yet others experience inconsistent patterns. This discrepancy raises important questions: Why does alcohol affect hot flashes differently among individuals? Is there a type of alcohol that exacerbates symptoms more than others? And most importantly, can reducing or eliminating alcohol help reduce hot flashes? This comprehensive guide explores the nuanced relationship between alcohol and hot flashes through the lens of perimenopause, helping you make informed, empowered decisions.
You may also like: Essential Tips for Managing Menopause: How to Stop Thyroid Hot Flashes Safely and Effectively
Understanding Perimenopause and the Onset of Hot Flashes
Perimenopause typically begins in a woman’s 40s, although it can start earlier or later depending on genetic, environmental, and lifestyle factors. It is characterized by fluctuations in estrogen and progesterone levels, leading to irregular menstrual cycles and a wide range of symptoms. One of the hallmark symptoms of this stage is the hot flash—a sudden sensation of intense heat, often accompanied by a flushed face, sweating, and sometimes heart palpitations or dizziness. These episodes can last anywhere from a few seconds to several minutes and may occur during the day or disrupt sleep at night, a phenomenon known as night sweats.
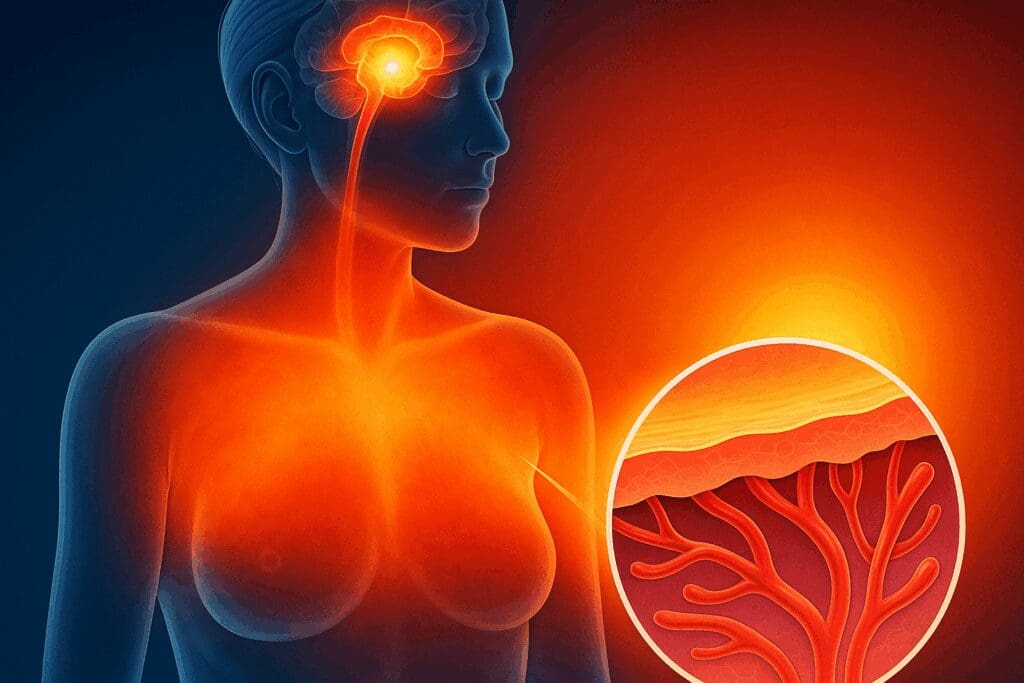
The precise mechanism behind hot flashes is not entirely understood, but research suggests that estrogen plays a critical role in regulating the hypothalamus, the part of the brain responsible for temperature control. When estrogen levels drop or fluctuate, this regulation becomes impaired, triggering vasodilation—or the widening of blood vessels—causing heat to dissipate through the skin and producing the sensation of a hot flash. Stress, caffeine, spicy foods, and alcohol are among the known external triggers that can exacerbate this process.
Alcohol and hot flashes intersect most noticeably through their shared impact on the body’s temperature regulation and hormonal balance. Ethanol—the active ingredient in alcoholic beverages—causes blood vessels to dilate, promoting heat loss and mimicking the vasomotor changes associated with hot flashes. This physiological overlap makes alcohol a particularly potent trigger during perimenopause.

The Science of Alcohol’s Impact on Hormones During Perimenopause
To fully appreciate the role of alcohol in hot flash frequency and severity, it is essential to understand how alcohol interacts with female hormones. Alcohol influences the endocrine system by altering the production, metabolism, and clearance of various hormones. Specifically, it has been shown to elevate estrogen levels transiently by affecting liver metabolism. For premenopausal and perimenopausal women, this can further destabilize an already fluctuating hormonal environment.
At low doses, alcohol might momentarily boost estrogen and produce a calming effect by increasing dopamine and serotonin. However, these short-lived benefits are quickly replaced by adverse outcomes. As the liver processes alcohol, it prioritizes ethanol metabolism over the breakdown of other compounds, including estrogen. This leads to a temporary surge in circulating estrogen, which can amplify the hormonal seesaw and intensify symptoms like hot flashes, mood swings, and sleep disturbances.
Further complicating matters, alcohol can reduce the body’s ability to manage cortisol and other stress hormones. During perimenopause, women are already more vulnerable to anxiety, irritability, and sleep disruption due to hormonal imbalances. Alcohol’s interference with the hypothalamic-pituitary-adrenal (HPA) axis—the body’s central stress response system—can exacerbate these issues, potentially making hot flashes more severe and frequent.

Perimenopause and Alcohol: Why Even Moderate Drinking Matters
Many women wonder whether occasional or moderate drinking is truly impactful. After all, a single glass of wine may seem harmless, and moderate alcohol use is often portrayed as socially acceptable or even beneficial in certain contexts. However, when it comes to perimenopause and alcohol, even small amounts can have disproportionate effects.
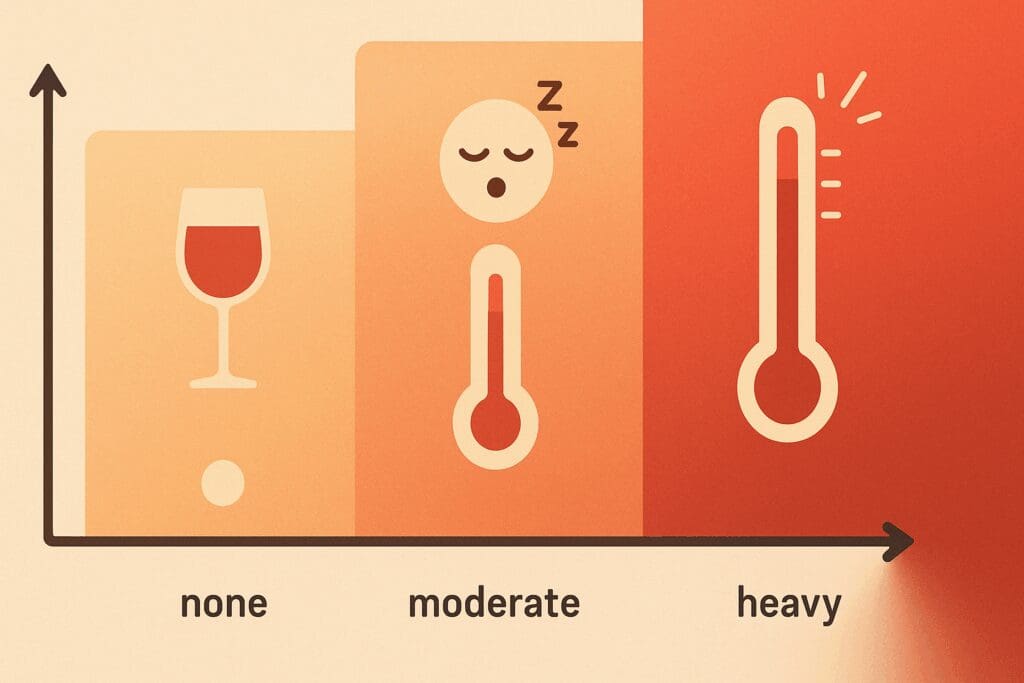
Studies have found that women who consume alcohol regularly report a higher frequency of hot flashes than those who abstain or drink rarely. This correlation exists regardless of the type of alcohol consumed, although red wine, with its higher concentration of congeners and histamines, is often cited as a particularly potent trigger. This does not necessarily mean that red wine is inherently worse than other alcoholic beverages, but rather that its composition can interact more strongly with the immune and vascular systems.
Moderate drinking also contributes to disrupted sleep patterns, a common complaint among perimenopausal women. Alcohol may initially promote drowsiness, but it reduces REM sleep and causes frequent awakenings during the second half of the night. This fragmented sleep exacerbates fatigue, irritability, and the perception of hot flashes as more distressing. Over time, what begins as a seemingly innocuous glass of wine with dinner can become a cycle of poor sleep, intensified hot flashes, and increased emotional stress.
Moreover, moderate alcohol intake is associated with changes in body temperature regulation, dehydration, and impaired thermoregulatory sweating—all of which can mimic or amplify the physical sensations of hot flashes. Given that perimenopausal bodies are already less efficient at maintaining temperature equilibrium, alcohol simply adds fuel to the fire.
Alcohol and Hot Flashes: What the Research Shows
Research into the relationship between alcohol and hot flashes reveals a consistent but complex picture. Observational studies have frequently reported a higher prevalence of hot flashes among women who consume alcohol, yet not all studies find a direct dose-response relationship. This inconsistency may be due to individual variations in genetic metabolism, hormone sensitivity, and liver function.
One prominent study published in the journal Menopause found that women who drank alcohol experienced more frequent and intense hot flashes compared to non-drinkers. Interestingly, this study also noted that women who drank heavily—defined as more than seven drinks per week—reported the highest rates of night sweats and sleep disruption. The findings underscore that not only does alcohol have a direct vasodilatory effect, but it may also contribute to systemic inflammation, which further destabilizes the body’s internal temperature regulation.
Additionally, alcohol is known to alter the gut microbiome and increase gut permeability, leading to low-grade inflammation. This inflammation can interfere with estrogen receptor activity and exacerbate vasomotor symptoms. Inflammatory markers such as C-reactive protein (CRP) and interleukin-6 (IL-6), often elevated in chronic alcohol users, have been linked to more severe menopausal symptoms, including hot flashes.
Despite these findings, not all women respond the same way to alcohol. Some may find that small amounts of white wine or beer do not trigger symptoms, while others experience severe hot flashes after a single drink. These differences highlight the importance of personal experimentation and awareness when managing symptoms.

Best Alcohol for Hot Flashes: Is There a Safer Option?
The idea of finding the “best alcohol for hot flashes” might seem paradoxical, but it’s a question many women ask when seeking to balance social enjoyment with symptom management. While no alcohol is entirely safe or symptom-free during perimenopause, some types may be less likely to provoke hot flashes than others.
White wine and clear spirits like vodka or gin generally contain fewer congeners—chemical byproducts of fermentation and aging that can irritate the nervous system and blood vessels. In contrast, red wine, dark liquors, and aged spirits tend to be higher in histamines and tannins, which can trigger histamine intolerance symptoms, including flushing, headaches, and heat intolerance.
That said, alcohol’s impact on hot flashes is not solely about the type of drink, but also about the quantity, timing, and personal sensitivity. Drinking on an empty stomach, during hot weather, or in combination with spicy food can heighten the vasodilatory effects of alcohol and increase the likelihood of experiencing a hot flash. Conversely, drinking slowly, staying hydrated, and eating protein-rich foods may reduce the intensity of symptoms.
Ultimately, the best alcohol for hot flashes may be no alcohol at all, especially for those who experience severe or frequent symptoms. However, for women who choose to drink, being selective about the type, limiting intake to one drink, and paying attention to body cues can help mitigate discomfort.
Why Does Alcohol Make You Hot? The Biological Mechanisms Explained
One of the most frequently asked questions among women in perimenopause is, “Why does alcohol make you hot?” The answer lies in how alcohol affects the body’s thermoregulatory and vascular systems. Alcohol acts as a vasodilator, which means it causes blood vessels, especially those near the surface of the skin, to expand. This widening allows more blood to flow near the skin, producing a sensation of warmth and often leading to flushing or sweating.
This mechanism is not unique to perimenopause; it can occur in anyone. However, during perimenopause, the hypothalamus—the brain’s temperature-regulating center—is already hypersensitive due to fluctuating estrogen levels. When alcohol enters the system and initiates vasodilation, the hypothalamus overreacts, misinterpreting the normal increase in heat as excessive. It responds by triggering the body’s cooling systems—namely, sweating and rapid heartbeat—hallmarks of a hot flash.
Additionally, alcohol disrupts the balance between excitatory and inhibitory neurotransmitters in the brain. This disruption affects autonomic functions, including those governing blood pressure, temperature regulation, and perspiration. The end result is a cascade of responses that mimic or amplify the experience of a hot flash, making it difficult to distinguish between alcohol-induced warmth and hormone-related episodes.
Even more telling is the consistency with which alcohol triggers hot flashes across diverse populations, age groups, and ethnic backgrounds. This widespread reaction underscores the universality of alcohol’s vasomotor effects, which become especially problematic during hormonally sensitive periods such as perimenopause.
Perimenopause and Alcohol: How to Stop Alcohol-Related Hot Flashes
Understanding how to stop alcohol hot flashes requires both lifestyle awareness and a willingness to experiment with personal boundaries. The first and most effective step is to reduce or eliminate alcohol consumption altogether, at least temporarily, to assess its impact on symptoms. Many women find that abstaining for just a few weeks yields noticeable improvements in both the frequency and intensity of hot flashes, as well as improved sleep and emotional stability.
For those not ready to quit entirely, consider adopting a harm-reduction approach. This could include choosing beverages with fewer additives, avoiding alcohol before bedtime, and always consuming alcohol with food to slow absorption. Keeping a symptom journal can also be helpful. Track what you drink, when you drink it, and how your body responds. Patterns may emerge that reveal specific triggers—such as certain types of alcohol, times of day, or even emotional states—that increase your vulnerability to hot flashes.
Hydration plays a critical role in minimizing alcohol-related symptoms. Because alcohol is a diuretic, it contributes to dehydration, which can amplify hot flashes by impairing the body’s cooling mechanisms. Countering this effect by drinking a glass of water between alcoholic beverages or increasing your overall fluid intake can make a significant difference. Likewise, adding electrolytes and anti-inflammatory foods such as leafy greens, berries, and omega-3-rich fish can support hormonal balance and reduce the inflammatory response to alcohol.
If hot flashes persist despite reducing alcohol, it may be worth exploring other contributing factors such as caffeine intake, stress, or poor sleep hygiene. Addressing these variables holistically will not only help manage hot flashes but also support broader hormonal health during perimenopause.
Alcohol and Menopause: Continuing Effects Beyond Perimenopause
While this article primarily focuses on perimenopause, it’s important to note that alcohol and menopause remain interconnected well beyond the transitional years. Even after periods cease and menopause is fully established, alcohol can continue to affect vasomotor symptoms, bone health, cardiovascular function, and emotional well-being.
In postmenopausal women, the liver’s capacity to metabolize alcohol often diminishes due to age-related changes, making the body more sensitive to smaller quantities of alcohol. Additionally, decreased estrogen levels mean the protective cardiovascular and skeletal benefits once attributed to this hormone are no longer present, leaving the body more vulnerable to alcohol’s negative effects. These include increased blood pressure, elevated triglycerides, and reduced bone density.
Women in menopause may also find that alcohol worsens urinary incontinence, vaginal dryness, or sleep disturbances. These symptoms can be mistakenly attributed solely to aging or hormonal decline, but alcohol’s exacerbating role is often overlooked. Furthermore, as estrogen levels remain consistently low post-menopause, the risk of systemic inflammation and oxidative stress rises—conditions that are both aggravated by regular alcohol consumption.
On a psychological level, alcohol use can mask underlying anxiety or depression, which are common during and after menopause. Because alcohol interferes with neurotransmitter production, particularly serotonin and dopamine, long-term use can actually deplete the brain’s natural capacity for mood regulation, leading to a cycle of dependence and emotional instability.
Thus, reevaluating alcohol consumption during menopause is not only about controlling hot flashes—it’s a broader issue of safeguarding overall health and emotional resilience as women age.
Why Do I Get Hot When I Drink Alcohol? Exploring Personal Sensitivity
The question “Why do I get hot when I drink alcohol?” is one that plagues many women, especially during perimenopause. The answer lies in individual sensitivity to alcohol’s byproducts, as well as genetic factors that influence alcohol metabolism. People of East Asian descent, for example, may experience alcohol flush reaction due to a deficiency in aldehyde dehydrogenase, an enzyme involved in alcohol breakdown. This genetic variation causes a buildup of acetaldehyde, leading to facial flushing, increased heart rate, and a sensation of internal heat.
Even outside of genetic predisposition, some individuals are simply more reactive to the effects of alcohol on blood vessels and body temperature. These people may feel hot, flushed, or dizzy after consuming relatively small amounts of alcohol, and this reaction tends to intensify during hormonal transitions. Women in perimenopause are particularly susceptible due to the estrogen-related changes in blood vessel elasticity and thermoregulation.
Certain ingredients in alcoholic beverages can also contribute to this reaction. Histamines, sulfites, and congeners commonly found in wine and beer can provoke immune responses that include flushing, itching, or increased warmth. These responses are often misinterpreted as “just a hot flash,” when in fact they represent a compound physiological effect triggered by specific substances in the drink.
Monitoring your individual response and becoming familiar with which types and amounts of alcohol provoke the strongest reactions can help you make more informed decisions. Some women may tolerate one small cocktail with dinner but find themselves overheating after a single glass of red wine. Personal experimentation, guided by awareness and curiosity rather than guilt or self-denial, is key to finding your unique tolerance threshold.
Does Alcohol Make You Hot? Debunking the Myths with Science
It’s a common anecdote: a glass of wine leads to a flushed face, a sweaty brow, or even a feeling of internal burning. So, does alcohol make you hot? The answer is yes, but the heat is misleading. While alcohol creates the sensation of warmth, it actually cools the body overall by promoting heat loss through the skin. This is why people who drink heavily in cold environments are at higher risk for hypothermia—they feel warm due to vasodilation, but their core temperature drops dangerously.
In the context of perimenopause and hot flashes, however, this false heat sensation is problematic. The body is already in a state of thermoregulatory confusion, and alcohol’s misleading signal can tip the scales toward a full-blown hot flash. This effect is particularly noticeable in women who are already dealing with hormonal instability, as alcohol compounds the internal chaos with external triggers.
Additionally, alcohol stimulates the release of norepinephrine and epinephrine—hormones that prepare the body for action by increasing heart rate and blood flow. While this might feel energizing in the short term, it contributes to the overall feeling of warmth and agitation. For perimenopausal women, these adrenal responses may intensify night sweats or create a spike in body heat that disrupts sleep.
Understanding that alcohol-induced warmth is not genuine heat production but rather a redistribution of existing heat can help women recognize why their bodies are reacting this way. This insight allows for more conscious decision-making around alcohol consumption, particularly in settings where heat intolerance is already a concern.

Perimenopause and Alcohol: Strategies for Symptom Relief and Lifestyle Balance
Living with perimenopausal symptoms doesn’t have to mean sacrificing all enjoyment. The goal is not necessarily total abstinence from alcohol, but rather achieving a sustainable balance that honors your body’s evolving needs. For many women, this means reframing their relationship with alcohol from one of routine to one of intention.
Start by identifying your motivation for drinking. Are you reaching for a glass of wine to unwind, to sleep, or to ease anxiety? If so, consider whether other tools—such as herbal teas, mindfulness practices, or journaling—might offer similar relief without the side effects. Replacing alcohol with calming rituals can create space for rest and reflection, which are particularly nourishing during perimenopause.
Support your body with nutrients that enhance liver function and hormonal health. Cruciferous vegetables like broccoli, kale, and Brussels sprouts contain compounds that aid in estrogen metabolism, while magnesium, vitamin B6, and omega-3 fatty acids support mood and neurotransmitter balance. Staying hydrated and exercising regularly will also help regulate body temperature, reduce stress, and promote better sleep—three essential components for managing hot flashes.
Finally, enlist support from your social circle. It can be challenging to navigate social settings that revolve around drinking, but having a few go-to phrases or non-alcoholic beverage alternatives can ease the transition. Many women find empowerment in setting boundaries, and discover that sobriety or moderation often inspires others to reevaluate their habits too.
Alcohol and Hot Flashes: A Holistic Perspective on Health and Hormones
Looking at alcohol and hot flashes through a holistic lens allows us to see the interplay of physiology, psychology, and lifestyle. Alcohol is not inherently evil, but its effects on the perimenopausal body are complex and often counterproductive to the goals of balance and well-being. By understanding the mechanisms behind alcohol’s impact and taking a proactive approach to symptom management, women can regain a sense of agency during a time that often feels unpredictable.
The perimenopausal journey is deeply individual, yet many of its challenges are universal. Whether you’re navigating night sweats, mood swings, or simply trying to understand why a glass of wine feels different than it did ten years ago, know that you’re not alone. With knowledge, compassion, and a willingness to adapt, you can create a lifestyle that supports your body’s transformation and enhances your quality of life.
Frequently Asked Questions: Understanding the Hidden Dynamics of Perimenopause and Alcohol
1. How does perimenopause affect how alcohol is metabolized in the body?
Perimenopause can significantly alter how the body processes alcohol due to hormonal fluctuations, especially involving estrogen and progesterone. These hormonal shifts can impact liver enzyme activity, making alcohol metabolism slower or more erratic than before. Many women notice that even a small amount of alcohol now leads to stronger or more prolonged effects. This altered metabolism also means an increased sensitivity to alcohol-related side effects, such as disrupted sleep, anxiety, and vasomotor symptoms like night sweats. These changes are particularly relevant when exploring the interaction between perimenopause and alcohol, as many symptoms attributed to menopause may actually be exacerbated by drinking patterns.
2. Why does alcohol make you hot during perimenopause—and does it ever get better?
The sensation of becoming flushed or overheated after drinking is common and often worsens during perimenopause. This is largely due to alcohol’s vasodilating effects, which expand blood vessels and raise skin temperature. During perimenopause, the body is already struggling to regulate temperature due to estrogen decline, making alcohol’s effects more intense. Women may find that even a single glass of wine triggers what feels like an exaggerated hot flash. If you’re asking, why does alcohol make you hot, the answer lies in the double impact of hormonal thermoregulation loss and alcohol’s direct influence on blood flow. The good news is that some women report gradual improvement post-menopause when hormones stabilize—although limiting intake still remains key.
3. What is the relationship between alcohol and hot flashes in different climates?
Interestingly, climate can amplify the connection between alcohol and hot flashes. In warmer, humid regions, alcohol’s vasodilatory effect can make hot flashes more severe and frequent due to already elevated core temperatures. Conversely, in cooler climates, alcohol-induced warmth might feel temporarily soothing, but it still triggers the same hormonal cascade leading to night sweats or sudden flushing. The environment may intensify symptoms, but the root problem remains the interplay between fluctuating estrogen and alcohol’s impact on thermoregulation. Women who travel often might find their symptoms worsen in certain environments, making it helpful to track their alcohol and hot flash symptoms geographically for better management.
4. How can someone figure out the best alcohol for hot flashes?
There’s no universal answer for the best alcohol for hot flashes, but patterns can be identified by tracking personal triggers. Clear spirits like vodka or gin, particularly when sugar-free and consumed with water or soda, are often better tolerated than red wine or sugary cocktails. Tannins in red wine and congeners in darker liquors can intensify vasomotor symptoms. Additionally, hydration status plays a key role—pairing every alcoholic drink with a glass of water may lessen symptom severity. Ultimately, it’s less about finding a magical drink and more about identifying the type and amount that causes the least disruption during perimenopause.
5. Why do some women feel anxiety after drinking during perimenopause?
The link between perimenopause and alcohol is not just physical—it’s also emotional. Estrogen has a calming effect on the brain, and its decline during perimenopause leaves many women more vulnerable to anxiety and mood swings. Alcohol, a depressant, may initially seem to reduce stress, but it often leads to a rebound effect that includes heightened anxiety, especially the day after drinking. This “hangxiety” is more pronounced during perimenopause because the nervous system is already dysregulated. Understanding this mechanism can help women make more informed decisions about drinking during this stage of life, especially if anxiety or sleep disturbances are prominent.
6. How to stop alcohol hot flashes without quitting drinking entirely?
If you’re wondering how to stop alcohol hot flashes without fully abstaining, there are several strategies that might help. First, reducing the volume and frequency of consumption can lessen symptom severity. Switching to drinks with fewer additives, avoiding sugary mixers, and spacing drinks out with water can help regulate body temperature. Timing also matters—avoiding alcohol in the evening may prevent overnight hot flashes and sleep disruption. Some women also benefit from taking natural supplements like black cohosh or evening primrose oil, though it’s important to consult with a healthcare provider before introducing new remedies. Moderation and strategic planning are often more sustainable than total abstinence.
7. Does alcohol and menopause affect sleep differently than before?
Yes, the relationship between alcohol and menopause has a marked effect on sleep architecture. Alcohol may help induce drowsiness initially, but it disrupts the second half of the sleep cycle, especially REM sleep, which is already compromised by hormonal shifts in menopause. This can lead to frequent awakenings, vivid dreams, or night sweats. Women who drink before bed are more likely to experience fragmented sleep, waking up tired despite a full night in bed. Understanding the compounding impact of alcohol on menopausal sleep issues can be the first step in reclaiming restorative rest through better lifestyle choices.
8. Why do I get hot when I drink alcohol even when I’m not drinking much?
The question why do I get hot when I drink alcohol often comes up among perimenopausal women who feel like they’re reacting more strongly to smaller amounts. This heightened sensitivity is due to a combination of slower alcohol metabolism, reduced estrogen, and increased blood vessel reactivity. Even half a glass of wine can cause facial flushing or a sudden hot flash-like sensation. For some, the reaction might be a sign of histamine intolerance or alcohol intolerance, which can become more noticeable during hormonal changes. It’s important not to dismiss these symptoms as normal aging, especially if they’re accompanied by dizziness, heart palpitations, or nausea.
9. How does social drinking change during perimenopause?
Navigating perimenopause and alcohol within a social context can be uniquely challenging. Many women feel pressure to continue drinking in social settings, even when their bodies are no longer tolerating it well. As alcohol starts to trigger symptoms like hot flashes, anxiety, or disrupted sleep, some women begin adjusting their routines—opting for mocktails, slower drinking, or fewer events centered on alcohol. There’s also a psychological shift: as perimenopause can bring heightened introspection and sensitivity, many become more aware of how alcohol affects their mood and confidence. Socializing doesn’t have to stop, but evolving your habits to align with your changing physiology is a powerful act of self-care.
10. What’s the future of research on alcohol and menopause?
As awareness of the intersection between alcohol and menopause grows, more research is focusing on gender-specific and age-specific responses to alcohol. New studies are exploring genetic factors that might make certain women more prone to alcohol-related hot flashes or sleep disruption. Hormone replacement therapy (HRT) and its interaction with alcohol is also an area of emerging interest, as it may modulate some negative effects. There’s a growing call for better clinical guidance that addresses the nuanced relationship between alcohol use and menopause transition. Future developments may include personalized health apps that track symptoms in relation to drinking, allowing for smarter, data-driven choices about alcohol use during this transformative stage.
Final Reflections: Reclaiming Comfort and Clarity Through Awareness of Perimenopause and Alcohol
In this essential stage of midlife, women deserve to feel empowered and informed. The connection between perimenopause and alcohol is both physiological and personal, shaped by hormonal flux, neurological responses, and lifestyle habits. As we’ve explored, alcohol can influence hot flashes by disrupting estrogen balance, compromising thermoregulation, and increasing systemic inflammation. While the experience of “getting hot” from alcohol is common, its impact during perimenopause is magnified, leading many women to reevaluate their relationship with drinking.
By addressing questions such as “why does alcohol make you hot” and “how to stop alcohol hot flashes,” this guide offers not just information but actionable strategies. Whether your goal is complete abstinence or mindful moderation, what matters most is your ability to listen to your body, honor its changing needs, and respond with informed choices. The path to comfort, clarity, and hormonal harmony begins with awareness—and continues with compassion for yourself as you navigate this transformative chapter.
Hot flashes are not just a nuisance; they are signals from your body asking for support. Whether that means reducing alcohol, changing your diet, or exploring new self-care routines, you have the tools—and now, the knowledge—to make changes that truly matter. And that, perhaps more than anything, is worth raising a (non-alcoholic) glass to.
Further Reading:
Mayo Clinic Minute: Why alcohol and menopause can be a dangerous mix
Hot Flush After Alcohol Consumption – What Does It Mean?



