Undergoing a hysterectomy marks a significant moment in a woman’s health journey, one often associated with complex emotional and physiological shifts. Among the most important long-term concerns is the effect of hysterectomy on bone integrity. Specifically, many women find themselves wondering how to prevent osteoporosis after hysterectomy—a critical question with implications that span decades of post-surgical life. As hormone levels shift and estrogen production declines, bone health becomes increasingly vulnerable, particularly for those who undergo early surgical menopause. Understanding how to actively maintain bone strength, prevent excessive mineral loss, and navigate the hormonal terrain that follows this procedure is vital not just for aging gracefully, but for preserving mobility, independence, and quality of life. This article offers a comprehensive, medically sound guide for preventing osteoporosis and supporting bone health in the years following a hysterectomy, especially for women who enter early menopause as a result.
You may also like: The Ultimate Guide to Meeting Your Nutritional Daily Requirements for Optimal Health

Understanding the Link Between Hysterectomy, Early Menopause, and Osteoporosis
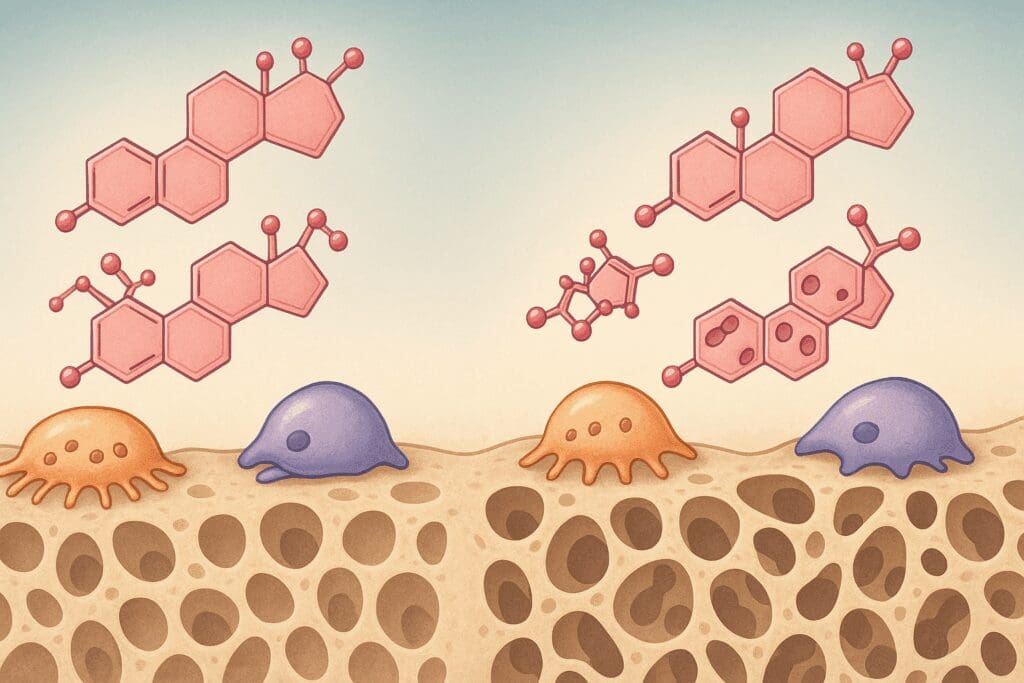
Hysterectomy, the surgical removal of the uterus, may also involve removal of the ovaries—a procedure known as oophorectomy—which triggers an abrupt onset of menopause. When this occurs before the natural menopausal age, the result is early menopause. The hormonal changes that accompany menopause, particularly the decline in estrogen, have a direct impact on bone remodeling. Estrogen plays a central role in maintaining bone density by regulating osteoclast activity—cells that break down bone tissue. With diminished estrogen, bone resorption outpaces bone formation, accelerating bone loss and elevating the risk of fractures.
Women who undergo early menopause and osteoporosis risk are inextricably linked. Studies reveal that women who experience menopause before age 45 are at significantly greater risk of developing low bone mineral density and sustaining fractures later in life. The situation becomes even more complex when early menopause is surgically induced. The body has no time to gradually adjust to hormonal shifts, which can lead to a more dramatic and immediate decline in bone mass. Therefore, understanding how menopause bone loss differs in women who’ve had a hysterectomy compared to natural menopause is crucial for formulating appropriate prevention strategies.
Osteoporosis, characterized by porous and fragile bones, remains one of the leading causes of disability in older women. Hip fractures, vertebral compression fractures, and decreased mobility are common consequences. For women in post-hysterectomy recovery, these outcomes are not inevitable. By recognizing how menopause bone density changes and how hysterectomy accelerates these changes, proactive measures can be taken to preserve skeletal strength and minimize lifelong risk.
Why Estrogen Matters: The Hormonal Foundation of Bone Health
The decline in estrogen following a hysterectomy with oophorectomy disrupts the body’s natural equilibrium of bone remodeling. This hormone not only modulates the activity of bone cells but also supports calcium absorption in the intestines and maintains the balance of calcium and phosphate in the bloodstream. With the loss of ovarian estrogen production, the delicate dance of bone resorption and formation tips in favor of breakdown.
It is important to understand the cascading physiological changes that occur in the absence of estrogen. Without its regulatory effect, osteoclast activity increases unchecked, leading to rapid deterioration of trabecular bone—the spongy, inner part of the bone that provides structural support. At the same time, osteoblasts—the cells responsible for building bone—become less effective, creating a double burden on bone mass retention.
This hormonal foundation explains why menopause and osteoporosis often go hand in hand, and it underscores the need for immediate, preventive intervention after a hysterectomy. To prevent osteoporosis, women should adopt lifestyle, nutritional, and medical strategies that directly address this hormonal void. While hormone replacement therapy (HRT) is one option, it is not the only path. Estrogen’s role provides a framework for selecting targeted interventions that aim to replicate or support its protective effect on bone.

How to Prevent Osteoporosis After Hysterectomy With Nutrition and Lifestyle Changes
Once the hormonal disruption begins, nutrition and lifestyle become the frontline defenses in preserving bone health. These modifiable factors can dramatically influence bone density trajectories and mitigate the risks associated with menopause bone loss. For women looking to understand how to prevent osteoporosis after hysterectomy, building a strong foundation with the right foods and habits is essential.
Calcium and vitamin D intake are paramount. Calcium provides the raw material for bone mineralization, while vitamin D enhances calcium absorption in the intestines and supports muscle function. Dairy products, leafy greens, fortified plant-based milks, and fish such as salmon and sardines offer rich sources of these nutrients. However, dietary intake alone may not suffice, especially when absorption is compromised with age. In such cases, high-quality supplements should be considered to meet the recommended daily allowances.
Beyond diet, physical activity is a powerful bone-preserving tool. Weight-bearing exercises like walking, hiking, dancing, and strength training create mechanical stress on bones, signaling the body to build and retain bone mass. Resistance training, in particular, improves muscle strength and balance, reducing the risk of falls and fractures. For women navigating menopause bone density loss, incorporating strength training at least two to three times a week is not optional—it’s a cornerstone of sustainable bone health.
In addition to calcium, other nutrients such as magnesium, vitamin K2, and protein play supporting roles in bone formation. Alcohol moderation and smoking cessation are also essential. Tobacco toxins directly impair osteoblast function, while alcohol reduces calcium absorption and affects hormone levels. Together, these lifestyle strategies form a holistic defense against menopause and osteoporosis.

Hormone Therapy and Non-Hormonal Alternatives for Bone Preservation
Hormone replacement therapy (HRT) remains a controversial yet potentially effective option for women seeking to prevent osteoporosis after menopause or hysterectomy. When used appropriately and under medical supervision, estrogen therapy can significantly slow bone loss and reduce fracture risk. For women under 60 or within 10 years of menopause onset, the benefits often outweigh the risks, especially for those at high risk of early menopause and osteoporosis.
HRT typically involves estrogen alone (for women without a uterus) or a combination of estrogen and progestin (for those who retain their uterus to protect the endometrium). The therapy works by restoring estrogen levels, thereby regulating bone resorption and preserving bone density. Numerous clinical trials demonstrate HRT’s effectiveness in maintaining lumbar spine and hip bone density, with some showing a reduction in vertebral fractures by up to 50%.
However, HRT is not suitable for everyone. For women with contraindications—such as a history of breast cancer, stroke, or clotting disorders—non-hormonal alternatives become essential. Selective estrogen receptor modulators (SERMs) like raloxifene mimic estrogen’s effect on bone while avoiding its risks in breast and uterine tissue. Bisphosphonates, another class of medications, reduce bone turnover and have been proven to decrease fracture risk in postmenopausal women.
Newer therapies, such as denosumab and parathyroid hormone analogs, offer alternative pathways for enhancing bone strength. These options are particularly useful for women with established osteoporosis or those who experience intolerable side effects from other treatments. The decision to use hormonal or non-hormonal therapy should be made collaboratively with a healthcare provider, considering personal health history, risk factors, and treatment goals.
Monitoring Bone Density: Early Detection as a Preventive Strategy
Bone mineral density (BMD) testing is a critical component of managing menopause and bone density loss, especially for women post-hysterectomy. Dual-energy X-ray absorptiometry (DEXA) scans offer precise measurements of bone mass in the hip and spine—areas most susceptible to osteoporotic fractures. For women seeking guidance on how to prevent osteoporosis after hysterectomy, regular BMD assessments allow for early detection of bone thinning and timely intervention.
Screening guidelines generally recommend that women begin BMD testing at age 65. However, women who undergo a hysterectomy with oophorectomy—particularly before age 50—should initiate testing much earlier. The abrupt decline in estrogen places them in a high-risk category, justifying more proactive monitoring. Baseline testing followed by periodic re-evaluation every one to two years enables clinicians to track changes, assess treatment efficacy, and adjust strategies as needed.
Monitoring tools extend beyond DEXA. Bone turnover markers in blood or urine can provide insight into the rate of bone resorption and formation, offering real-time feedback on how interventions are working. When used in conjunction with imaging, these markers enhance the precision of osteoporosis prevention efforts.
Early identification of bone loss is not merely a diagnostic exercise—it is a call to action. When BMD results indicate osteopenia (low bone mass) or osteoporosis, timely adjustments in lifestyle, nutrition, or pharmacological interventions can prevent progression and minimize fracture risk. In this sense, screening serves as a foundational pillar in the effort to prevent osteoporosis after menopause or surgical menopause.
Personalized Risk Assessment and Genetic Factors in Bone Health
Bone health is influenced by more than just surgery and hormones; genetics, ethnicity, and individual risk profiles also play substantial roles. Understanding these variables allows for a more nuanced approach to prevention and empowers women to take ownership of their skeletal well-being.
Family history remains one of the most reliable predictors of osteoporosis risk. Women whose mothers or grandmothers experienced fractures or were diagnosed with osteoporosis are more likely to face similar challenges. Genetic polymorphisms in genes related to collagen production, vitamin D receptor function, and calcium metabolism can also affect bone quality and responsiveness to treatment. These heritable traits underscore the importance of early screening and aggressive intervention in high-risk individuals.
Ethnicity further influences risk, with Caucasian and Asian women exhibiting a higher incidence of osteoporosis compared to African American and Hispanic women. However, no group is immune, and lifestyle factors can significantly modulate risk across all populations. For women wondering how to improve bone density during menopause, personalized risk assessment tools like the FRAX calculator can help estimate 10-year fracture risk based on age, weight, lifestyle, and medical history.
Medical comorbidities also factor in. Conditions like rheumatoid arthritis, thyroid disorders, chronic kidney disease, and gastrointestinal malabsorption syndromes can accelerate bone loss. Certain medications, including glucocorticoids, aromatase inhibitors, and some antiepileptic drugs, also compromise bone density. Identifying and managing these secondary risk factors is essential for a comprehensive prevention strategy.
Incorporating risk assessment into routine care ensures that osteoporosis prevention is not a one-size-fits-all endeavor. Instead, it becomes a targeted, strategic effort grounded in the realities of each woman’s biology and history.
How to Prevent Osteoporosis After Hysterectomy Through Targeted Supplementation
In the absence of sufficient estrogen, and even when dietary habits are optimal, supplements play a vital role in the long-term strategy to preserve bone strength after hysterectomy. Knowing how to prevent osteoporosis after hysterectomy often involves a careful selection of vitamins and minerals that not only enhance bone formation but also support overall hormonal balance and skeletal metabolism.
Calcium supplements remain a primary recommendation, especially for women whose dietary intake falls below the recommended 1,200 mg daily threshold for postmenopausal individuals. However, not all calcium sources are created equal. Calcium citrate is more bioavailable than calcium carbonate and is less dependent on stomach acid for absorption, making it an ideal choice for older adults. Taking calcium in divided doses throughout the day further enhances uptake and minimizes gastrointestinal discomfort.
Vitamin D3 is essential to accompany calcium supplementation. It promotes calcium absorption in the gut and ensures that it is deposited into bone tissue rather than remaining in circulation or contributing to vascular calcification. Most women require between 800 to 2,000 IU of vitamin D3 daily, depending on baseline levels and sun exposure. Blood tests can determine whether levels are adequate or whether more aggressive dosing is needed.
Other vital nutrients include magnesium, which aids in bone structure and is often deficient in modern diets, and vitamin K2, which helps direct calcium into bones rather than soft tissues. Collagen supplements are gaining recognition for their role in improving bone matrix quality, particularly in the trabecular bone affected most by estrogen deficiency. Strontium, boron, and trace minerals such as zinc and manganese also support bone metabolism, though these should be taken under professional guidance to avoid imbalances.
For women seeking to understand how to prevent osteoporosis after menopause, these supplements can serve as valuable tools, provided they are used strategically. It’s not merely about taking a multivitamin—it’s about targeting deficiencies that compromise bone regeneration and ensuring each nutrient is present in the right form, dose, and combination.

Psychological and Emotional Health: The Overlooked Component of Bone Wellness
While much of the discussion around menopause and osteoporosis focuses on physiology, the emotional and psychological dimensions cannot be ignored. Stress, depression, and anxiety are known to affect hormonal balance, appetite, motivation for physical activity, and even immune function—all of which indirectly impact bone health.
Cortisol, the body’s primary stress hormone, has a catabolic effect on bone tissue. Chronic elevations in cortisol can stimulate bone resorption and suppress osteoblast activity. For women undergoing the profound transition of a hysterectomy—often accompanied by feelings of loss, altered identity, or fear about aging—psychological stress can exacerbate the very physiological pathways that threaten bone health.
Moreover, depression often leads to reduced physical activity and poor dietary habits. This creates a harmful feedback loop where emotional struggles reduce the engagement in bone-protective behaviors. Addressing mental health is therefore not a luxury, but a necessity in any comprehensive plan to improve bone density during menopause and after hysterectomy.
Mind-body practices such as yoga, tai chi, and meditation not only reduce stress but also provide gentle, weight-bearing movement that enhances balance, flexibility, and proprioception. These activities are particularly effective at reducing fall risk and are ideal for women who may not tolerate more intensive exercise.
Therapy, support groups, and counseling also serve a vital role. Creating emotional resilience can empower women to stay proactive in their health journey and feel less overwhelmed by the multitude of decisions involved in osteoporosis prevention. A psychologically sound approach makes it far more likely that a woman will adopt and maintain the lifestyle changes that are necessary to preserve bone strength over time.

Fall Prevention and Environmental Safety: Practical Applications for Everyday Life
Even with strong bones, one bad fall can lead to a fracture that dramatically changes the course of a woman’s life. When menopause bone density declines and bones become brittle, the stakes are even higher. Therefore, one of the most immediate and practical ways to prevent osteoporotic injury is by minimizing fall risk.
Home modifications can have a profound impact. This includes installing grab bars in bathrooms, ensuring adequate lighting throughout the home, securing loose rugs, and adding non-slip mats in areas prone to wetness. Stairs should have sturdy railings on both sides, and cluttered pathways should be cleared regularly. These seemingly small changes create a safer living environment and significantly reduce the risk of falls.
Footwear also plays a role. Supportive, non-slip shoes help stabilize posture and prevent missteps. Women with declining vision or balance issues should consider mobility aids or occupational therapy evaluations to improve spatial awareness and coordination. Falls often result from a combination of minor impairments that accumulate over time; addressing them early makes prevention much more effective.
Exercise contributes to fall prevention beyond strengthening bones. It enhances muscle tone, joint stability, and neuromuscular control. Balance training—such as standing on one leg, heel-to-toe walking, or using balance boards—should be a part of every woman’s weekly routine. For those at higher risk, physical therapists can design personalized programs to improve gait, stability, and functional strength.
Falls are not merely accidents; they are often predictable and preventable. Women looking for ways to protect their bones after hysterectomy should consider fall prevention strategies just as essential as calcium supplements or hormone therapy. It is a daily practice rooted in awareness, preparation, and proactive self-care.
How to Prevent Osteoporosis After Hysterectomy by Embracing a Long-Term Mindset
The transition into menopause—especially surgical menopause—requires not only immediate adjustments but also a lifelong commitment to bone-preserving behaviors. Women who succeed in minimizing osteoporosis risk do so not through a one-time intervention but by adopting a mindset that embraces bone health as a sustained priority.
This mindset involves being vigilant yet not fearful. It means viewing bone health as part of overall wellness, not as an isolated issue. Just as one monitors cardiovascular health through regular check-ups and lifestyle choices, bone health should be tracked, supported, and adjusted over time. This includes ongoing dialogue with healthcare providers about changing needs as one ages.
Preventing osteoporosis is not only about avoiding fragility; it is about preserving strength, resilience, and the ability to live fully and independently. Every choice—from walking in the park instead of watching television, to opting for a calcium-rich meal over processed convenience food—compounds over time. The sooner these choices become habits, the more powerful their protective effect.
Women should not wait for signs of bone loss to take action. By the time fractures occur, the underlying disease is already advanced. Instead, prevention must begin at the first sign of hormonal changes—or better yet, before. Understanding how to prevent osteoporosis after menopause or hysterectomy is the first step; living that knowledge daily is where transformation truly begins.
Bone health is also dynamic. What worked at age 45 may need revisiting at 55 or 65. Hormonal status, activity levels, medications, and comorbidities change, and so must the strategies. Periodic reevaluation, curiosity, and willingness to adapt are hallmarks of successful long-term prevention.
FAQ: How to Prevent Osteoporosis After Hysterectomy – Expert Insights for Long-Term Bone Health
1. Why does a hysterectomy increase the risk of osteoporosis, especially in women under 50?
Women who undergo a hysterectomy, particularly with ovary removal, often experience a sudden drop in estrogen levels. This abrupt transition can simulate early menopause and osteoporosis, accelerating bone loss more rapidly than the gradual process of natural menopause. Even in cases where the ovaries are preserved, disruptions in blood flow may impair hormone production, indirectly contributing to menopause bone density reduction. This risk becomes more pronounced when hysterectomy occurs before age 50, shortening the window of natural estrogen protection. Women in this category should start early monitoring and proactive management to counteract the impact of menopause and bone density loss before it becomes clinically significant.
2. What are lesser-known lifestyle changes to support bone health post-hysterectomy?
In addition to calcium and vitamin D, several underutilized lifestyle shifts can help prevent osteoporosis after hysterectomy. Adopting a diet rich in magnesium, potassium, and vitamin K2—found in leafy greens and fermented foods—can enhance calcium metabolism and bone matrix formation. Avoiding long sedentary periods and opting for frequent micro-movements throughout the day—such as standing desk use or yoga stretches—improves skeletal loading and circulation. Mindful practices like meditation may also lower cortisol, a stress hormone that accelerates menopause bone loss. These holistic strategies work synergistically to stabilize hormonal fluctuations and enhance long-term menopause bone integrity.
3. How does early menopause after hysterectomy differ from natural menopause in terms of bone loss?
The hormonal descent in early menopause and osteoporosis cases is steep and unbuffered by the body’s usual adaptation time. This often results in more severe and faster menopause bone loss, with up to 20% of bone mass potentially lost within the first five years. Unlike natural menopause, which gives women time to adapt to waning estrogen, surgical menopause offers no such grace period. This sharp decline can also disrupt other systems like insulin sensitivity and inflammatory response, indirectly contributing to menopause and osteoporosis. For these reasons, hormone monitoring and customized interventions are crucial for women entering early menopause post-hysterectomy.
4. What role does resistance training play in reversing menopause-related bone loss?
Progressive resistance training doesn’t just maintain—it can actually reverse mild to moderate menopause bone density decline. Compound exercises such as squats, deadlifts, and step-ups activate multiple muscle groups and load major skeletal areas. These movements promote osteoblast activity, encouraging bone regeneration at a cellular level. When combined with adequate protein intake and vitamin D, weight-bearing exercises become a frontline defense to prevent osteoporosis women should prioritize. Notably, this form of training also reduces the risk of falls by improving balance, coordination, and muscular strength, critical for postmenopausal women.
5. What are the psychological and emotional impacts of post-hysterectomy bone loss?
The emotional toll of menopause and osteoporosis is often underrecognized. Women may experience anxiety about fracture risk, reduced mobility, or feelings of premature aging—especially following a sudden post-hysterectomy estrogen crash. This psychological strain can lead to lower physical activity, poor nutrition choices, and sleep disruption, which all negatively affect menopause bone health. Engaging in support groups or cognitive-behavioral therapy can help mitigate these feelings and empower patients to reclaim agency over their health. Addressing emotional well-being is as essential as physical interventions to prevent osteoporosis women should view care as mind-body integrated.
6. Can hormone replacement therapy (HRT) significantly reduce osteoporosis risk after hysterectomy?
Yes, HRT can be highly effective in mitigating the effects of menopause and bone density loss, especially for women under 60 or within 10 years of menopause onset. Estrogen therapy directly counteracts the skeletal weakening that accelerates after hysterectomy-induced menopause. However, therapy must be individualized based on personal and family history of cancer, cardiovascular disease, and clotting disorders. For many, transdermal patches or low-dose bioidentical hormone options provide a safer route to prevent osteoporosis after hysterectomy without elevating systemic risks. Long-term compliance and regular bone density testing are essential to maximize benefit while minimizing adverse effects.
7. How to improve bone density during menopause without medication?
How to improve bone density during menopause naturally involves a multi-pronged strategy. First, adopt an alkaline-promoting diet with anti-inflammatory foods like berries, fatty fish, and legumes, which reduce the body’s need to leach calcium from bones. Next, include exercises like jumping or jogging, which add mechanical stress to bones and stimulate osteogenesis. Certain botanical supplements, such as red clover and black cohosh, have phytoestrogenic effects and may offer mild protection against menopause and osteoporosis. Mindfully managing alcohol, caffeine, and tobacco exposure is also essential for maintaining optimal menopause bone density. Finally, ensure regular DEXA scans to track progress and adjust strategies as needed.
8. What advanced bone health biomarkers should women monitor post-hysterectomy?
Traditional bone density scans are useful but not always sensitive to early change. Emerging biomarkers can offer deeper insight to prevent osteoporosis women should act on before irreversible loss occurs. These include serum C-telopeptide (CTX), which measures bone resorption rate, and Procollagen type I N-terminal propeptide (P1NP), which indicates bone formation. A high CTX-to-P1NP ratio may suggest accelerated menopause bone loss, even when bone mineral density appears normal. Tracking these markers can help fine-tune interventions—whether dietary, hormonal, or lifestyle-based—and provide a more dynamic view of how to improve bone density during menopause.
9. How to prevent osteoporosis after hysterectomy with nutritional timing and absorption?
Strategic nutrient timing plays a critical role in maximizing calcium bioavailability and enhancing menopause bone resilience. For instance, spacing calcium and magnesium supplements apart can prevent competition in absorption. Pairing vitamin D with healthy fats, such as avocado or olive oil, boosts its effectiveness in facilitating calcium uptake into bone. Nighttime supplementation with magnesium may help counteract nocturnal bone resorption, which tends to spike during sleep. These advanced approaches reflect a more nuanced strategy to prevent osteoporosis women should incorporate into daily routines, especially post-hysterectomy when absorption efficiency may be altered.
10. How to prevent osteoporosis after menopause through long-term strategic planning?
How to prevent osteoporosis after menopause is not a one-time fix but a decades-long process of strategic decisions. Women should build a care team including a gynecologist, endocrinologist, and nutritionist who collaborate on a personalized bone health plan. Periodic reevaluation of lifestyle habits, lab results, and bone scan data is essential to adjust for changing needs across the aging spectrum. Investing in fall-proof home environments, from non-slip flooring to handrails, becomes increasingly important with age. Most importantly, fostering a proactive mindset and educating oneself on the evolving science of menopause and osteoporosis ensures long-term skeletal integrity. This comprehensive approach empowers women to retain mobility, independence, and quality of life well into their later years.
Summary and Final Reflections: Preserving Strength and Preventing Osteoporosis for a Healthier Future
For women navigating life after a hysterectomy, bone health is not just a concern—it is a central pillar of well-being. Understanding how to prevent osteoporosis after hysterectomy involves far more than just taking calcium tablets. It requires a multi-faceted, personalized, and proactive approach that integrates hormonal awareness, strategic supplementation, dietary excellence, physical activity, and emotional resilience.
Menopause and osteoporosis are undeniably intertwined, and the sudden hormonal shifts following surgical menopause demand urgent attention. Whether the concern lies in early menopause and osteoporosis risk or the general loss of menopause bone density, the principles of prevention remain clear: support the body through every available avenue—nutritional, medical, and lifestyle-based.
When it comes to how to improve bone density during menopause, knowledge must be paired with action. Weight-bearing exercises stimulate osteogenesis, while vitamin D and calcium provide the materials necessary for that growth. Hormonal therapies, when appropriate, restore the physiological balance needed to slow down resorption. Meanwhile, mindfulness and mental health support ensure that women are emotionally equipped to sustain these changes across the lifespan.
To prevent osteoporosis, women should remain informed, engaged, and consistent. No single strategy guarantees immunity from bone loss, but together, these measures form a powerful, protective network. By embracing the knowledge of menopause bone changes and taking deliberate, medically sound action, women can reduce their risk, improve their quality of life, and maintain their independence for years to come.
Ultimately, bone health after hysterectomy is about more than avoiding fractures—it is about preserving the foundation upon which a vibrant, active, and fulfilling postmenopausal life can be built. With the right tools, mindset, and support, every woman has the power to protect her bones and her future.



