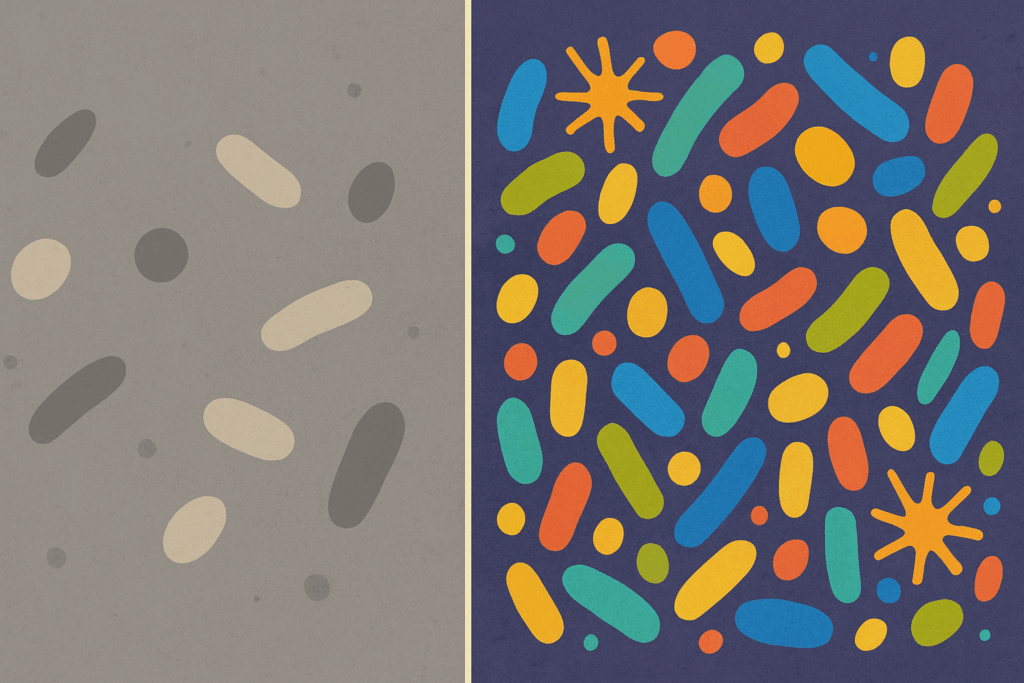
The intricate ecosystem within our digestive tract, commonly referred to as the gut microbiome, is a dynamic and essential component of human health. This delicate balance of microorganisms affects not only digestion but also immune function, mental well-being, and even metabolic efficiency. In recent years, increasing research has underscored the importance of learning how to rebuild gut microbiome health following illness, antibiotic use, poor dietary choices, or chronic stress. A restored and flourishing gut microbiome contributes significantly to long-term wellness, making it a central pillar of any health-optimized lifestyle.
Understanding how to rebuild gut microbiome strength begins with recognizing the signs of an unhealthy gut. Bloating, irregular bowel movements, chronic fatigue, mood disturbances, and skin issues may all point to imbalances in the microbiota. Modern life often assaults this vital system through over-processed foods, environmental toxins, and sedentary behaviors. However, the body possesses a remarkable capacity for renewal, particularly when supported by gut healing foods, lifestyle adjustments, and mindful dietary choices.
You may also like: The Ultimate Guide to a Healthy Balanced Diet for Women at Every Life Stage

The Science Behind Gut Microbiome and Digestive Health
The gut microbiome consists of trillions of bacteria, fungi, viruses, and other microorganisms that reside mainly in the colon. Each person’s microbial profile is unique, shaped by genetics, birth method, diet, environment, and lifestyle. These microorganisms are not passive inhabitants; rather, they interact actively with the host’s immune system, regulate digestion, produce vital nutrients such as vitamin K and certain B vitamins, and protect against pathogens.
When this microbial community is in balance, it fosters a healthy gut environment that supports nutrient absorption and intestinal integrity. However, disruptions can lead to a condition known as dysbiosis. This imbalance is often associated with symptoms of poor gut health, such as inflammation, increased intestinal permeability (leaky gut), and heightened susceptibility to infections. Restoring harmony within this ecosystem is not a matter of quick fixes; it requires a comprehensive understanding of how to heal your gut naturally through evidence-based practices.
Scientific evidence also suggests that the gut-brain axis plays a profound role in mental health, linking microbiome composition to mood, stress response, and even cognitive function. As such, the pursuit of gut health extends beyond digestive comfort to broader systemic effects, making it all the more crucial to know how to improve gut microbiome resilience and vitality.

Recognizing the Symptoms of Poor Gut Health
Identifying an unhealthy gut is the first step toward restoration. While digestive symptoms are the most direct indicators, the impact of gut imbalance can manifest in surprising ways. Symptoms of poor gut health include chronic bloating, gas, diarrhea, or constipation, all of which indicate that the digestive system is under stress. These symptoms are often overlooked or normalized but should be viewed as signals of a deeper imbalance.
Beyond the digestive tract, an impaired gut can influence systemic inflammation, manifesting in joint pain, autoimmune flare-ups, and skin conditions such as eczema or acne. Individuals with unhealthy gut symptoms may also experience frequent illness due to a weakened immune system. Mental health challenges such as anxiety and depression have also been linked to dysbiosis, suggesting that the microbiome plays a role in neurotransmitter production and mood regulation.
Moreover, cravings for sugar or processed foods may indicate a disrupted microbiota, as pathogenic bacteria often thrive on these dietary patterns. Understanding these multifaceted signs allows individuals to take a proactive approach to healing by learning how to fix gut microbiome imbalances through diet and lifestyle interventions.
Why Is Gut Health Important for Overall Wellness?
The significance of gut health extends beyond digestion and nutrient absorption. The gut acts as a major interface between the body and the external environment, playing a central role in immune surveillance and systemic regulation. Nearly 70% of the body’s immune cells reside in the gastrointestinal tract, highlighting its role as an immunological hub.
A healthy gut microbiome contributes to the production of short-chain fatty acids (SCFAs) like butyrate, which nourish colon cells, reduce inflammation, and support gut barrier integrity. These metabolites are critical for maintaining a robust internal environment that protects against chronic diseases such as inflammatory bowel disease, type 2 diabetes, and cardiovascular conditions.
Furthermore, the gut-brain connection reveals that gut health is integral to emotional regulation and cognitive performance. Serotonin, a neurotransmitter often associated with mood, is predominantly produced in the gut. Therefore, addressing gut health may provide an avenue for improving mental clarity, reducing stress, and supporting emotional balance.
Understanding how to restore gut microbiome function is essential not only for managing symptoms but for promoting vitality, resilience, and long-term health. Through intentional choices in nutrition and lifestyle, it is possible to build a gut environment that enhances well-being on every level.

Essential Dietary Shifts for Gut Repair and Microbiome Restoration
Food is one of the most powerful tools available for transforming gut health. The best diet for gut health is one that emphasizes variety, plant-based nutrients, and fiber-rich whole foods. These dietary components feed beneficial microbes and promote microbial diversity, which is a hallmark of a resilient microbiome.
Including prebiotic foods such as garlic, onions, leeks, and asparagus provides fuel for probiotic bacteria, encouraging their growth and activity. Fermented foods like kefir, sauerkraut, kimchi, and yogurt introduce live cultures that help repopulate the gut with beneficial strains. These gut healthy foods offer both immediate support and long-term benefits for intestinal harmony.
Avoiding processed sugars and refined carbohydrates is equally important, as these substances feed harmful bacteria and contribute to dysbiosis. A gut health diet should also limit artificial sweeteners and preservatives, which have been shown to alter microbial balance. Instead, nutrient-dense, anti-inflammatory foods such as leafy greens, berries, wild-caught fish, and olive oil support healing and resilience.
Hydration is another critical component of gut repair. Water supports the mucosal lining of the intestines and facilitates the elimination of waste, allowing the gut environment to remain clean and functional. When considering how to heal your gut microbiome, prioritizing hydration is a simple yet impactful step.
How to Rebuild Gut Microbiome After Antibiotic Use
Antibiotics, while life-saving, are known to significantly disrupt the gut microbiota by eliminating both harmful and beneficial bacteria. This disruption can result in reduced microbial diversity and increased vulnerability to opportunistic infections such as Clostridium difficile. Knowing how to rebuild gut microbiome health post-antibiotic use is essential for recovery.
Replenishing the gut with high-quality probiotics can help restore microbial populations. Selecting multi-strain supplements with clinically studied species such as Lactobacillus and Bifidobacterium provides targeted support. However, probiotics are most effective when paired with a diet rich in prebiotic fibers that sustain their growth.
Time and patience are also key. The gut microbiome does not bounce back overnight. It can take weeks or even months to fully recover microbial diversity and functionality. During this period, consistent dietary support, reduced stress, and sufficient sleep can all accelerate the healing process.
Ultimately, rebuilding the microbiome post-antibiotics is not merely about replacing what was lost but creating an environment where beneficial microbes can flourish. This involves not just supplementation but a comprehensive gut reset that emphasizes whole-food nutrition, mindful eating, and sustainable lifestyle practices.

How to Heal Your Gut Naturally Through Lifestyle Practices
Beyond dietary interventions, lifestyle factors play a significant role in determining gut health. Chronic stress has been shown to negatively impact the gut barrier and alter microbial composition. Engaging in regular stress-reduction techniques such as mindfulness meditation, breathwork, and gentle exercise can significantly enhance gut function.
Sleep also influences the gut microbiome. Disrupted sleep patterns have been linked to increased intestinal permeability and reduced microbial diversity. Prioritizing consistent sleep hygiene—including regular bedtimes, dark sleep environments, and minimal blue light exposure—can support microbial equilibrium and gut repair.
Physical activity has systemic benefits, including the modulation of gut flora. Moderate, consistent movement such as walking, yoga, or strength training has been associated with improved microbial diversity and increased SCFA production. These effects underscore the importance of incorporating movement into any plan aimed at learning how to improve gut health naturally.
Social connection and emotional well-being also influence gut health. Positive social interactions reduce stress hormones and promote parasympathetic nervous system activity, which enhances digestion. Building meaningful relationships and fostering emotional resilience is therefore a surprising yet vital aspect of restoring gut health.
Gut Healing Foods That Promote Microbial Balance
The path to a healthy gut is paved with nutrient-dense foods that nourish the microbiome and support the intestinal lining. Certain foods possess exceptional gut-healing properties and should be incorporated regularly into the diet.
Bone broth, for instance, is rich in collagen, glutamine, and glycine—compounds that help repair intestinal walls and reduce inflammation. Its soothing texture makes it especially beneficial during periods of active gut distress. Similarly, omega-3 fatty acids found in fatty fish like salmon and sardines possess anti-inflammatory effects that promote microbial stability.
Colorful vegetables and fruits supply polyphenols, which are plant compounds with prebiotic-like effects. Berries, green tea, and cocoa are examples of polyphenol-rich foods that selectively enhance the growth of beneficial bacteria. These compounds act as natural modulators of the gut environment, shaping microbial communities in favorable ways.
Fiber is another cornerstone of a healthy gut diet. Soluble and insoluble fibers found in oats, legumes, chia seeds, and root vegetables provide both bulk and fermentable substrates for gut bacteria. These fibers improve bowel regularity and increase the production of SCFAs, promoting gut integrity and reducing systemic inflammation.

How to Rebuild Gut Microbiome with Long-Term Dietary Strategies
Rebuilding the microbiome is not a short-term project; it requires sustainable dietary patterns that nourish and protect microbial diversity over time. Emphasizing whole, minimally processed foods is the foundation of such a strategy.
Rotational eating, or varying food choices from week to week, prevents the dominance of any single bacterial species and fosters a diverse microbial ecosystem. This approach supports long-term adaptability and resilience, especially when paired with seasonal, local produce that introduces a range of microbial exposures.
Reducing the intake of emulsifiers, additives, and pesticides also contributes to gut health. Choosing organic options and reading ingredient labels can minimize chemical exposures that disrupt microbial harmony. These conscious food choices serve as both preventive and restorative tools in microbiome care.
When contemplating how to reset gut microbiome health, meal timing may also play a role. Intermittent fasting or time-restricted eating has been shown to influence microbial composition and enhance intestinal repair processes. Incorporating overnight fasting windows of 12–14 hours can offer a reset period for the gut.
Ultimately, the best diet for gut health is one that is personalized, balanced, and nutrient-rich. Whether addressing existing imbalances or maintaining optimal function, these dietary principles lay the groundwork for enduring digestive vitality.
Understanding Different Gut Types and Individualized Healing Approaches
Not all guts are the same, and recognizing different gut types can guide individualized strategies for improvement. Some people may have fast transit times, characterized by frequent bowel movements and nutrient malabsorption, while others may experience sluggish digestion and chronic constipation.
Identifying your gut type helps tailor interventions to your unique needs. For instance, someone with a “sensitive” gut may require a more gradual introduction of fiber and fermented foods, while another with a more resilient system may benefit from bolder dietary experimentation. Testing for microbial diversity, food sensitivities, and digestive enzymes can offer deeper insights into individual gut function.
A personalized approach ensures that the focus remains on how to heal your gut naturally without triggering additional inflammation or discomfort. Working with a nutritionist or functional medicine practitioner can provide targeted guidance based on lab results, symptoms, and lifestyle factors.
The emerging field of microbiome testing continues to provide tools for precision wellness. By understanding specific bacterial strains and imbalances, individuals can take a more strategic approach to restoring balance and preventing future disruptions. This personalized path reinforces the principle that gut healing is a journey, not a one-size-fits-all solution.
How to Improve Gut Microbiome Through Supplementation and Herbal Support
While food remains the cornerstone of gut health, supplements can offer concentrated support during critical periods of healing. Probiotics and prebiotics are often the first line of defense, but other nutrients and herbs also play pivotal roles.
Digestive enzymes can assist in breaking down food more efficiently, reducing the burden on an inflamed or underperforming digestive system. These enzymes can be particularly helpful for individuals with pancreatic insufficiency or gallbladder removal. L-glutamine, an amino acid, supports intestinal wall repair and is commonly used in gut repair protocols.
Herbs such as slippery elm, marshmallow root, and licorice provide mucilaginous compounds that coat and soothe the intestinal lining. These traditional remedies have been validated by modern science and are especially helpful in cases of leaky gut or irritable bowel syndrome.
It’s important to approach supplementation with care and professional guidance. Not all products are created equal, and dosages matter. Integrating these supports into a broader strategy on how to heal your gut microbiome enhances their effectiveness and ensures long-term benefits.
Rebuilding Gut Microbiome for Long-Term Health and Prevention
A resilient gut microbiome is one that adapts, recovers, and protects against future disruptions. Once the immediate imbalances have been addressed, the focus should shift to maintenance and prevention. Consistency in dietary and lifestyle habits ensures that the gains achieved are not lost over time.
Mindful eating, characterized by chewing thoroughly, eating without distraction, and paying attention to hunger cues, supports both digestion and microbial balance. These practices reduce the likelihood of overeating, improve nutrient absorption, and enhance satisfaction with meals.
Continued diversity in food choices prevents microbial stagnation, while seasonal cleansing practices such as short-term elimination diets or gut resets can offer occasional tune-ups. These periodic efforts help recalibrate the system and reinforce the foundation of a healthy gut.
Learning how to increase gut health over the long term is about integration rather than perfection. Small daily choices, such as starting the day with a fiber-rich smoothie or ending with a relaxing walk, contribute to an overall lifestyle that honors the gut’s role in total wellness.
Frequently Asked Questions on Gut Health and Microbiome Restoration
How does travel affect gut health, and what can you do to protect your microbiome?
Travel often exposes individuals to unfamiliar foods, water sources, and time zones, all of which can disrupt the gut microbiome. Jet lag can impair the body’s circadian rhythm, which plays a regulatory role in digestive processes and microbial activity. Moreover, abrupt changes in diet, especially a reduction in fiber or increase in processed foods while traveling, may lead to symptoms of poor gut health such as bloating or irregularity. To protect your microbiome during travel, consider packing shelf-stable gut healthy foods like chia seeds, dried fruit, and prebiotic-rich snacks. Staying hydrated, maintaining consistent meal timing, and taking a quality probiotic during and after your trip can help restore balance and support gut repair.
What are the most promising trends in how to rebuild gut microbiome research?
Recent research is exploring the potential of personalized nutrition based on individual microbiome profiles to inform how to rebuild gut microbiome health. Scientists are developing targeted probiotics that adapt to specific gut types, enhancing efficacy compared to one-size-fits-all supplements. Additionally, fecal microbiota transplantation (FMT), once reserved for severe conditions like C. difficile infection, is now being studied as a therapeutic option for other gut-related disorders. Postbiotics—metabolites produced by beneficial microbes—are gaining attention as a novel way to mimic the effects of probiotics without live organisms. These developments signal a future where gut health interventions are precise, personalized, and grounded in genomic analysis.
Can emotional health influence symptoms of poor gut health?
Yes, emotional health plays a significant role in gut function and microbial balance. Chronic stress and anxiety activate the hypothalamic-pituitary-adrenal (HPA) axis, increasing cortisol levels and altering the gut lining’s permeability. This disruption can lead to unhealthy gut symptoms such as discomfort, constipation, or diarrhea. Emerging studies show that practicing mindfulness, engaging in social support, and even cognitive behavioral therapy can positively influence the gut-brain axis. A holistic approach that combines emotional wellness with a gut health diet has shown to be especially effective for those learning how to heal your gut naturally.
What advanced testing options exist to identify the best diet for gut health?
Beyond general dietary advice, advanced microbiome testing can analyze the composition of your gut flora to recommend the best diet for gut health specific to your microbial profile. These tests measure the abundance of beneficial vs. harmful bacteria and assess how well your body metabolizes various food groups. Some platforms now use AI-driven insights to generate personalized food plans that focus on gut healing foods tailored to your biology. Other tests measure inflammatory markers, digestive enzyme activity, and even fungal overgrowth. For individuals seeking a more data-driven approach to how to fix gut microbiome issues, these diagnostics can offer actionable insights beyond traditional food logs or symptom diaries.
How to rebuild gut microbiome after long-term medication use (not just antibiotics)?
While antibiotics are well-known for disrupting gut flora, other long-term medications—including proton pump inhibitors, NSAIDs, and antidepressants—can also impair microbial balance. These drugs may alter stomach acidity, mucus production, or bile flow, all of which impact gut types and bacterial diversity. To support microbiome recovery, focus on reintroducing gut healthy foods high in polyphenols, like artichokes and blueberries, which help rebalance microbial populations. Incorporating fermented vegetables, bone broth, and resistant starches into a healthy gut diet can further assist with gut reset. Gradual reduction of unnecessary medications under medical supervision, along with functional nutrition support, can accelerate how to restore gut microbiome integrity over time.
What are some underestimated lifestyle factors that affect gut health?
Many people overlook the impact of light exposure and screen time on gut health. Disruption of circadian rhythms due to late-night screen use can desynchronize gut microbiota cycles and impair digestion. Similarly, inadequate physical movement reduces gut motility, leading to symptoms of poor gut health such as bloating and constipation. Air quality also plays a role, with research suggesting that exposure to pollutants can alter microbial balance and promote inflammation. Creating a daily routine that includes outdoor activity, natural light exposure, and digital detoxes can offer subtle but powerful support to how to improve gut health naturally. Such changes also align well with gut repair strategies that target both physical and emotional health.
What does a successful gut reset look like, and how long does it typically take?
A gut reset typically involves eliminating inflammatory foods, increasing gut healing foods, and introducing lifestyle changes that support microbial diversity. Initial results, such as improved bowel movements or reduced bloating, can be seen within a week, but full microbial restoration often takes 8 to 12 weeks. During this time, consistency is key. People aiming for how to reset gut microbiome balance should avoid common setbacks such as yo-yo dieting, overuse of cleanses, or excessive supplementation. Success is marked by improved digestion, better energy levels, reduced cravings, and diminished symptoms of poor gut health. Monitoring changes in mood, sleep, and skin health can also provide valuable indicators of progress.
How to rebuild gut microbiome in children and adolescents?
Children and teens have unique gut types that are still developing, making early interventions especially impactful. Diets high in processed snacks and low in fiber can quickly disrupt microbial balance during these formative years. Introducing gut healthy foods like kefir smoothies, lentil soups, and vegetable-rich stews can make a substantial difference. Physical activity and outdoor play expose children to diverse environmental microbes, which can positively influence their microbiota. Parents focused on how to improve gut microbiome health in younger individuals should also consider limiting antibiotic use to medically necessary situations and encouraging mindful eating habits from an early age.
Are there seasonal approaches to gut repair or maintenance?
Yes, syncing your diet and lifestyle to seasonal rhythms can enhance how to heal your gut microbiome. In colder months, warming gut healing foods such as bone broth, root vegetables, and cooked greens are beneficial for soothing digestion and supporting immunity. Spring and summer offer an abundance of prebiotic-rich fruits and raw vegetables, which can aid in gut reset and refresh microbial diversity. Seasonal variation also helps expose your body to different environmental microbes, fostering adaptability in the gut ecosystem. Aligning meal timing with natural daylight and incorporating seasonal herbs like dandelion or nettle tea can further enhance how to heal your gut naturally.
What long-term strategies can help prevent the return of unhealthy gut symptoms?
Preventing the recurrence of symptoms requires an ongoing commitment to a gut health lifestyle rather than short-term fixes. Regularly consuming the best foods for gut health—such as high-fiber vegetables, fermented products, and omega-3-rich fish—helps maintain microbial balance. Periodic check-ins with a healthcare provider can catch early signs of poor gut health before they escalate. Incorporating a once-a-week fast, community meals, and minimal screen time after dinner are strategies that reinforce how to fix microbiome resilience over time. Understanding that gut health is dynamic encourages proactive habits that make how to increase gut health a sustainable, enjoyable process.
The Takeaway: Why Rebuilding the Gut Microbiome Is Vital to Your Health Journey
Restoring and maintaining gut health is one of the most impactful steps an individual can take toward holistic well-being. Knowing how to rebuild gut microbiome function equips you with the tools to influence not only digestion but immunity, mental clarity, and disease prevention. The journey is not linear, but every intentional step matters.
From recognizing the symptoms of poor gut health to embracing a gut health diet rich in whole foods and supportive nutrients, the path to healing is grounded in both science and self-awareness. Integrating personalized strategies, mindful lifestyle habits, and evidence-based supplementation creates an environment in which the microbiome can thrive.
As research continues to unfold, the connection between gut health and systemic wellness becomes increasingly clear. Investing in your gut is an investment in your future—a daily act of care that yields compounding returns. Whether you are recovering from illness, managing chronic symptoms, or simply striving for optimal vitality, your microbiome holds the key to transformative change.
Embrace the process, seek professional guidance when needed, and stay curious. With time, commitment, and the right information, your gut can become your greatest ally in the pursuit of lifelong health.



