Introduction: A New Mother’s Silent Battle and the Role of Zoloft
Becoming a mother is often described as one of life’s most transformative experiences, rich with wonder, emotional depth, and profound love. Yet for many women, this new chapter also ushers in unexpected emotional challenges that can cloud the joy of early motherhood. Among the most common and under-discussed issues faced during the postpartum period is postpartum anxiety, a condition that affects an estimated 10% to 15% of new mothers worldwide. Despite its prevalence, postpartum anxiety remains overshadowed by its more widely recognized counterpart, postpartum depression. In recent years, increasing attention has been given to the role of pharmacological interventions—particularly selective serotonin reuptake inhibitors (SSRIs)—in managing postpartum mental health. One such SSRI, sertraline, more commonly known by its brand name Zoloft, has emerged as a frequently prescribed option. This article offers breakthrough insights on Zoloft for postpartum anxiety: what every new mom should know, from how it works and when it’s appropriate to the science behind its use and its potential side effects.
The emotional and psychological well-being of new mothers is a critical component of both maternal and infant health. When left unaddressed, postpartum anxiety can affect bonding, sleep, lactation, and overall family dynamics. With stigma gradually receding and discussions around maternal mental health becoming more normalized, understanding the clinical nuances and lived experiences surrounding treatments like Zoloft is essential. This article aims to bridge the gap between clinical evidence and compassionate care, offering medically accurate, SEO-optimized, and empathetically delivered information for mothers, partners, and healthcare providers alike.
You may also like: Essential Tips for Navigating Emotional and Physical Changes at 8 Months Postpartum

Understanding Postpartum Anxiety: More Than Just the “Baby Blues”
Postpartum anxiety is distinct from the fleeting emotional shifts commonly referred to as the “baby blues.” While the baby blues typically involve mood swings, tearfulness, and irritability that resolve within two weeks of delivery, postpartum anxiety is characterized by persistent, excessive worry that interferes with a mother’s ability to function. These worries often center around the health and safety of the baby, but can also extend to broader concerns such as financial instability, household management, or personal adequacy as a parent. Physical symptoms—racing heart, nausea, dizziness, and insomnia—can mimic other medical conditions, making diagnosis particularly challenging.
Clinically, postpartum anxiety can manifest in several forms, including generalized anxiety disorder (GAD), panic disorder, obsessive-compulsive disorder (OCD), and even post-traumatic stress disorder (PTSD), especially in mothers who have experienced traumatic labor or delivery. Each subtype presents unique symptoms but shares a core element: a heightened, often uncontrollable sense of worry. Unfortunately, societal expectations that portray motherhood as innately fulfilling can lead many women to hide their distress, fearing judgment or feeling guilty for not meeting perceived ideals. This suppression not only delays treatment but may exacerbate symptoms over time.
The biological underpinnings of postpartum anxiety involve a complex interplay of hormonal fluctuations, sleep deprivation, and pre-existing mental health conditions. Estrogen and progesterone levels drop dramatically after childbirth, and this hormonal withdrawal is believed to influence neurotransmitter systems in the brain, including serotonin—the key chemical targeted by SSRIs like Zoloft. Understanding these dynamics is crucial to appreciating why pharmacological interventions may be warranted, particularly when lifestyle modifications and talk therapy alone prove insufficient.
How Zoloft Works in the Brain and Why It’s Often Recommended
Zoloft (sertraline) belongs to the class of medications known as selective serotonin reuptake inhibitors. It works by inhibiting the reabsorption (or reuptake) of serotonin in the brain, thereby increasing its availability in the synaptic cleft—the space between neurons where communication occurs. Serotonin is a neurotransmitter implicated in mood regulation, emotional stability, and cognitive function. By boosting serotonin levels, Zoloft helps mitigate the persistent worry, agitation, and physiological arousal that characterize postpartum anxiety.
One reason Zoloft is frequently prescribed for postpartum anxiety is its favorable safety profile, especially during lactation. Several studies have shown that sertraline is excreted in breast milk at low levels, with minimal detectable levels in infant plasma. These findings suggest that the medication poses minimal risk to breastfeeding infants, although careful monitoring is always advised. The American Psychiatric Association and the American College of Obstetricians and Gynecologists both list Zoloft among the first-line treatments for perinatal mood and anxiety disorders due to this safety profile.
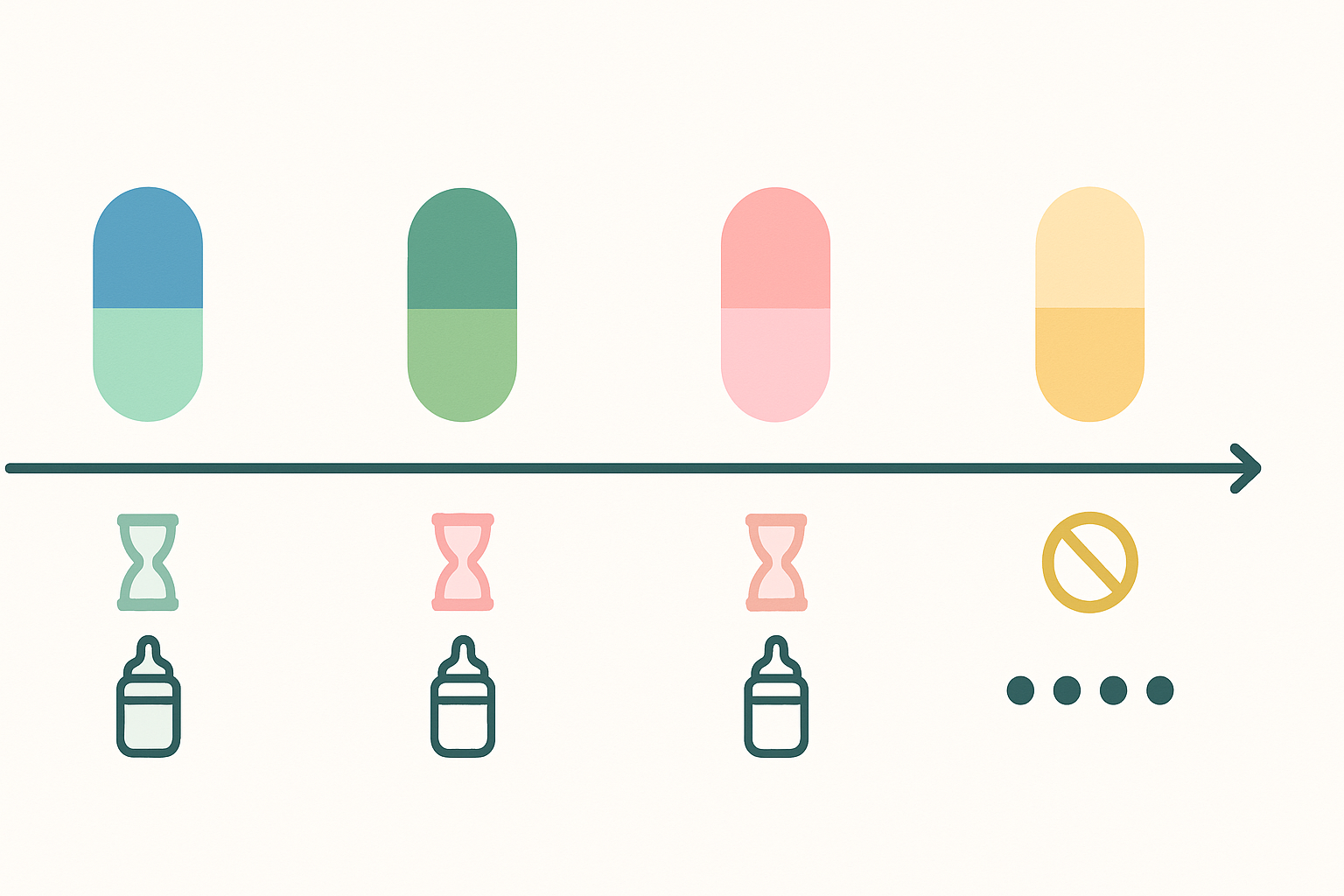
Moreover, Zoloft’s efficacy in reducing anxiety symptoms has been well documented in broader populations, and although fewer randomized controlled trials focus specifically on postpartum women, existing data and clinical consensus support its utility. The medication typically takes 4 to 6 weeks to exert noticeable effects, though some mothers report improvements earlier. It’s important to emphasize that Zoloft is not a “quick fix,” but rather one component of a comprehensive mental health strategy that may also include therapy, peer support, and lifestyle adjustments.
Breakthrough Insights on Zoloft for Postpartum Anxiety: What Every New Mom Should Know About Effectiveness
When considering Zoloft for postpartum anxiety, the most pressing question for many mothers is: “Will it work for me?” Effectiveness is not a one-size-fits-all metric but must be evaluated within the context of symptom severity, coexisting conditions, and individual neurobiology. Clinical studies suggest that SSRIs, including Zoloft, are effective in reducing the frequency and intensity of anxiety symptoms, improving sleep, and enhancing daily functioning. However, effectiveness can vary based on how early treatment is initiated and whether the mother adheres to the prescribed regimen.
One breakthrough insight involves the synergistic role of psychotherapy in enhancing Zoloft’s efficacy. Cognitive-behavioral therapy (CBT), for example, complements the pharmacological action of SSRIs by helping mothers identify distorted thinking patterns and develop more adaptive coping strategies. In many cases, the combination of Zoloft and CBT leads to faster and more sustained symptom reduction compared to either treatment alone. This dual approach also empowers mothers to regain a sense of control and agency, which can be especially meaningful in the emotionally turbulent postpartum period.
Another often overlooked aspect is the importance of dosage titration. Zoloft is typically started at a low dose (e.g., 25mg daily) to minimize side effects, and then gradually increased based on tolerance and therapeutic response. Some mothers may require higher doses (up to 100-200mg daily) for optimal results. The need for individualized dosing underscores the importance of regular follow-ups with a healthcare provider who can adjust the regimen as needed. Patience and communication are key—what works for one mother may not work for another, and adjustments should be expected as part of the treatment journey.
Navigating the Side Effects and Managing Expectations
As with any medication, Zoloft comes with potential side effects, though many are transient and subside within the first few weeks of treatment. Common side effects include nausea, fatigue, dry mouth, dizziness, and changes in appetite. In some cases, women report initial increases in anxiety or restlessness, which can be disconcerting but are usually temporary. Healthcare providers often recommend taking the medication with food and during the evening to mitigate nausea and sleep disturbances. If side effects persist or become intolerable, switching to a different SSRI or adjusting the dosage may be necessary.
More serious but rare side effects include serotonin syndrome—a potentially life-threatening condition resulting from excessive serotonin activity—and suicidal ideation, particularly in younger individuals. While these outcomes are uncommon, they warrant vigilance, especially during the first few weeks of treatment. It’s essential for mothers and their families to be aware of warning signs and to maintain open lines of communication with healthcare professionals.
A vital aspect of managing expectations is understanding that Zoloft is not a cure, but a tool. It does not eliminate life’s stressors or guarantee an absence of worry. Instead, it aims to create a more stable emotional baseline from which mothers can better engage in daily life, form stronger bonds with their babies, and pursue therapy or self-care routines more effectively. Setting realistic goals—such as improved sleep, better mood regulation, and reduced panic episodes—can help mothers evaluate progress and remain motivated throughout the treatment process.
Breakthrough Insights on Zoloft for Postpartum Anxiety: What Every New Mom Should Know About Risks and Benefits
The decision to start Zoloft involves a careful risk-benefit analysis, especially during a period as delicate as postpartum recovery. On the one hand, untreated postpartum anxiety can have serious consequences, not just for the mother but also for the infant’s emotional and cognitive development. Chronic maternal anxiety has been linked to difficulties with breastfeeding, disrupted attachment, and developmental delays in infants. From this perspective, the potential benefits of symptom relief and emotional stabilization are compelling.
On the other hand, concerns about side effects and long-term dependency often weigh heavily on mothers’ minds. While Zoloft is not addictive in the traditional sense—it does not cause cravings or require escalating doses to achieve the same effect—discontinuation can lead to withdrawal symptoms such as dizziness, irritability, and flu-like sensations. For this reason, any plan to stop the medication should be done gradually and under medical supervision. The concept of “tapering off” is crucial and should be discussed early in the treatment process to alleviate fears about long-term commitment.
It’s also worth noting that Zoloft is one of the few SSRIs that has been extensively studied in lactating women, and its low transfer rate into breast milk offers an added layer of reassurance for nursing mothers. For women who are not breastfeeding, the treatment landscape may offer additional flexibility in terms of dosage and adjunctive medications. In both scenarios, informed decision-making grounded in evidence, rather than fear or stigma, should guide the process.
How Zoloft Compares to Other SSRIs in Postpartum Treatment
While Zoloft for postpartum anxiety is a leading choice among healthcare providers, it’s important to understand how it compares to other SSRIs like fluoxetine (Prozac), paroxetine (Paxil), and citalopram (Celexa). Each of these medications functions similarly in boosting serotonin levels, but they differ in half-life, side-effect profiles, and safety considerations—especially in the context of breastfeeding and postpartum recovery. Zoloft’s short half-life means it exits the body relatively quickly, which can be advantageous when managing side effects or transitioning off the medication. It also means that missed doses may be more noticeable, requiring greater adherence to a consistent dosing schedule.
Compared to fluoxetine, which has a significantly longer half-life and may linger in both maternal and infant systems for an extended period, Zoloft is often preferred for nursing mothers. Paroxetine, though effective for anxiety, has been associated with higher rates of withdrawal symptoms upon discontinuation and may not be the first-line choice during lactation. Meanwhile, citalopram and escitalopram (Lexapro) share similar effectiveness but may carry a slightly different risk profile in terms of cardiac side effects and require close monitoring in patients with a family history of heart conditions.
Ultimately, the decision to prescribe Zoloft over other SSRIs hinges on a combination of factors: the mother’s medical history, prior response to medications, current symptoms, and breastfeeding status. In collaborative care models, this decision is made jointly between the mother, her obstetrician, and, if applicable, a psychiatrist. This team-based approach ensures that the treatment plan reflects not just clinical guidelines but also the mother’s personal values and goals.
Breakthrough Insights on Zoloft for Postpartum Anxiety: What Every New Mom Should Know About Emotional Healing
One of the more nuanced and powerful insights about using Zoloft for postpartum anxiety is the way it facilitates—not replaces—emotional healing. While medication can reduce the acute intensity of anxiety symptoms, true recovery often involves coming to terms with the profound psychological adjustments that accompany motherhood. For many women, the transition to motherhood brings up unresolved fears, insecurities, or past trauma, and these must be addressed through supportive dialogue, not just chemical intervention.
In this context, Zoloft can be seen as a bridge—a stabilizing force that enables mothers to engage more fully in therapy, process complex emotions, and develop coping skills that will serve them beyond the postpartum period. For example, a mother struggling with intrusive thoughts may find that after a few weeks on Zoloft, she has the mental bandwidth to explore these thoughts in therapy without being overwhelmed by them. In other cases, mothers report feeling more present and capable of enjoying bonding moments with their baby once the relentless undercurrent of anxiety is alleviated.
Moreover, the psychological impact of choosing to take medication can itself be therapeutic. For some mothers, initiating Zoloft represents an act of self-compassion—a declaration that their mental health matters and that they deserve to feel well. This shift in mindset can catalyze a broader reevaluation of self-worth and priorities, setting the stage for a more sustainable approach to motherhood. The stigma surrounding psychiatric medication, especially in the context of new motherhood, is slowly dissolving, and embracing pharmacological help can be a bold and empowering step toward healing.

Zoloft and Postpartum Depression: Dual Benefits and Overlapping Symptoms
It’s not uncommon for postpartum anxiety and postpartum depression to occur simultaneously, and many mothers may find themselves struggling with both conditions in varying degrees. Fortunately, Zoloft for postpartum depression is also widely prescribed, making it a versatile option for mothers with mixed presentations. The medication’s dual efficacy lies in its modulation of serotonin, which affects both mood and anxiety regulation. By alleviating the low mood, fatigue, and hopelessness characteristic of depression while also tempering the restlessness and worry of anxiety, Zoloft offers a comprehensive approach to postpartum mental health.
Recognizing the overlapping symptoms between these two conditions is crucial. For instance, difficulty sleeping, irritability, and difficulty concentrating can be signs of either depression or anxiety, or both. Misdiagnosis or underdiagnosis can lead to suboptimal treatment and prolonged suffering. Healthcare providers are increasingly aware of these nuances and are trained to conduct thorough assessments that distinguish between the various postpartum mood disorders. In this setting, Zoloft’s broad-spectrum utility is particularly valuable, as it can address a range of symptoms without requiring multiple medications.
For mothers who initially seek treatment for postpartum depression and later discover that anxiety is a more dominant concern, staying on Zoloft often remains an effective strategy. Its gradual and cumulative effect on neurochemical balance allows for symptom evolution and adjustment over time. Moreover, treating one set of symptoms often alleviates others indirectly—for example, improved sleep due to reduced anxiety can enhance mood, and better mood can reduce catastrophic thinking. This interconnectedness highlights the benefit of a unified treatment approach.
The Role of Partners and Family in Supporting Treatment
Support from partners and family members can significantly influence a mother’s decision to seek and adhere to treatment. Postpartum anxiety can be isolating, and the idea of taking psychiatric medication may evoke feelings of shame or weakness—emotions that are often compounded by societal expectations of maternal self-sacrifice. In such cases, validation from a trusted partner can make a meaningful difference. Statements like “I see how much you’re struggling, and I support whatever you need to feel better” can be more healing than any medical advice.
Family members can also assist by normalizing treatment, helping with childcare during therapy appointments, or even participating in couples or family therapy. Understanding the purpose and mechanism of Zoloft can dispel myths or fears about personality changes or emotional blunting. In reality, many mothers report feeling more like themselves on Zoloft, not less. By alleviating the fog of constant worry, the medication often allows their true personality to shine through more clearly.
It’s also important for support networks to understand that recovery is not linear. There may be days of relapse, emotional setbacks, or even decisions to adjust or switch medications. Rather than interpreting these changes as failures, partners and families should view them as part of the dynamic process of healing. Patience, empathy, and informed engagement can transform treatment from a solitary act into a shared journey.
Tapering Off: How to Safely Transition Away from Zoloft
At some point, many mothers wonder when—and how—they might stop taking Zoloft. Tapering off is a deeply personal decision that should be guided by symptom stability, life stressors, and professional input. It is generally advised to wait at least six months to a year before considering tapering, particularly if the initial symptoms were severe. Premature discontinuation can lead to relapse, often more intense than the original episode. Therefore, a gradual reduction in dosage, supervised by a healthcare provider, is essential.
The tapering process typically involves reducing the dose in small increments every few weeks, monitoring for withdrawal symptoms or the re-emergence of anxiety. Some mothers find it helpful to concurrently increase therapy sessions during this time or to adopt new stress-management techniques such as mindfulness, journaling, or physical exercise. These strategies can provide an emotional buffer during the transition and reinforce the gains made while on medication.
It’s also crucial to understand that returning to medication is not a sign of defeat. Some women may need to resume Zoloft during subsequent pregnancies or periods of high stress, and that’s entirely valid. The goal is not to prove resilience by enduring without help but to cultivate a toolkit that includes both pharmacological and non-pharmacological options. Whether Zoloft becomes a short-term aid or a longer-term anchor, its role is ultimately to support a mother’s capacity to thrive.
Frequently Asked Questions: Advanced Insights on Zoloft for Postpartum Anxiety and Related Conditions
How does Zoloft interact with hormonal changes after childbirth?
The postpartum period is marked by significant hormonal fluctuations, particularly the sharp drop in estrogen and progesterone, which can destabilize neurotransmitter systems. Zoloft, by increasing serotonin availability, may help buffer the emotional fallout caused by these hormonal shifts. While it doesn’t directly affect hormone levels, it does help regulate mood and anxiety responses that become dysregulated in the aftermath of hormonal withdrawal. Interestingly, some research suggests that SSRIs like Zoloft may indirectly influence the hypothalamic-pituitary-adrenal (HPA) axis, potentially modulating the stress response in postpartum women. Understanding this interaction is crucial because it highlights that Zoloft not only addresses symptoms but may help recalibrate biological systems destabilized during childbirth.
Can Zoloft improve maternal-infant bonding in cases of postpartum anxiety or depression?
Yes, emerging studies and clinical observations suggest that treating postpartum anxiety and depression with Zoloft can positively affect mother-infant bonding. When maternal mental health is impaired, bonding often suffers due to emotional withdrawal, irritability, or intrusive thoughts. By alleviating these symptoms, Zoloft can make mothers more emotionally available and responsive to their infants’ cues. While the medication doesn’t directly enhance bonding, it removes emotional obstacles that hinder it. Some therapists also incorporate parent-infant interaction therapy alongside pharmacological treatment to reinforce healthy attachment, creating a more comprehensive approach to healing.
Is Zoloft for postpartum anxiety equally effective for women with a history of generalized anxiety disorder?
Zoloft has demonstrated consistent efficacy across various anxiety disorders, including generalized anxiety disorder (GAD), and this remains true in the postpartum context. Women with a preexisting history of GAD may even respond more quickly to Zoloft, as their brains may already be primed for SSRI responsiveness. However, they may also require longer courses of treatment or higher doses, especially if their baseline anxiety was already elevated before pregnancy. For such individuals, continuity of care is key—many providers recommend continuing Zoloft during pregnancy if it was previously effective, thereby minimizing postpartum relapse. Regular psychiatric follow-up is essential to ensure that both perinatal and general anxiety symptoms are adequately addressed.
What are some lifestyle modifications that enhance the effects of Zoloft in postpartum treatment?
Several lifestyle interventions can enhance the effectiveness of Zoloft for postpartum anxiety and depression. Regular physical activity, even low-intensity walks with the baby, can improve mood and support serotonin function. Mindfulness practices such as meditation or deep breathing exercises help retrain the brain’s stress responses, offering a complementary benefit to pharmacotherapy. Adequate nutrition, especially maintaining blood sugar balance and consuming foods rich in omega-3 fatty acids, can further support neurological stability. Social support also plays a pivotal role; joining postpartum support groups, whether virtual or in-person, provides a nonjudgmental environment for shared experiences and emotional validation. These non-pharmacologic strategies should be viewed as allies in the healing process rather than replacements for medication.
How does Zoloft influence sleep quality in mothers with postpartum depression or anxiety?
One of the paradoxes of Zoloft and postpartum is that while the medication ultimately improves sleep by reducing anxiety, it can initially disrupt sleep due to activating side effects. Some mothers report vivid dreams or difficulty falling asleep during the first few weeks of treatment. However, as Zoloft reaches steady-state levels in the bloodstream, these side effects often resolve, and overall sleep quality improves as anxiety diminishes. Better sleep in turn contributes to faster emotional recovery, reduced irritability, and improved physical healing. It’s helpful for mothers to establish sleep hygiene routines during the adjustment period and to work closely with providers to optimize dosage timing—often taking Zoloft in the morning mitigates night-time restlessness.
Is there a preferred time to initiate Zoloft for postpartum anxiety—during pregnancy or after birth?
This question depends on the mother’s mental health history and symptom severity. Initiating Zoloft during the third trimester is becoming more common among women with high-risk mental health profiles, particularly those with prior episodes of major depression or severe anxiety. This preemptive approach can reduce the likelihood of a full-blown postpartum crisis. For others, symptoms may only emerge postnatally, at which point starting Zoloft as soon as symptoms interfere with functioning is generally advised. Obstetric psychiatrists often use a risk-benefit analysis to determine timing, with consideration of breastfeeding goals, social support, and past medication responses. This proactive decision-making exemplifies how integrated, anticipatory care is essential in modern maternity mental health practices.
How do cultural perceptions influence the decision to use Zoloft for postpartum anxiety?
Cultural beliefs play a significant role in shaping attitudes toward mental health and medication use during the postpartum period. In some cultures, seeking psychiatric care may be stigmatized, and Zoloft may be viewed with suspicion due to concerns about dependency or personality changes. Others may view emotional struggles as signs of spiritual imbalance or familial shame, discouraging open discussion and treatment. These beliefs can delay diagnosis and reduce adherence to prescribed medication. For clinicians and family members, cultural sensitivity is key—open conversations that validate the mother’s feelings while gently introducing evidence-based treatment options can bridge the gap between cultural norms and medical best practices. Involving community leaders or bilingual support workers can also facilitate more inclusive care.
Breakthrough Insights: What makes Zoloft for postpartum anxiety stand out from other treatments?
Zoloft stands out from other treatments for postpartum anxiety due to its dual emphasis on efficacy and safety—particularly during breastfeeding. Its favorable pharmacokinetics, including a short half-life and low transfer rate into breast milk, make it a top choice among SSRIs for nursing mothers. In addition to its biochemical compatibility, Zoloft also offers psychological advantages. Women who take it often report a feeling of emotional stability without sedation or dullness, making it easier to engage in parenting tasks and therapeutic activities. Unlike benzodiazepines, which may work more quickly but risk dependency and sedation, Zoloft offers a sustainable and safe option for long-term recovery. Its clinical reputation continues to grow as more studies confirm its benefits in diverse postpartum populations.
What are the long-term emotional effects of staying on Zoloft for postpartum depression or anxiety?
For some women, long-term use of Zoloft becomes part of an integrated mental health plan that supports emotional resilience well beyond the postpartum period. Rather than dulling emotions, Zoloft is reported to enable a fuller range of emotional experiences by reducing overwhelming anxiety or depressive flatness. Over time, the clarity and stability it provides can help women rebuild self-trust and develop lasting coping skills. Psychologists often observe that women who stay on Zoloft for longer durations are more likely to make meaningful progress in therapy, suggesting that medication can act as a foundation for deeper psychological work. Long-term use should still be periodically reassessed, but many women find that continuing the medication gives them a reliable tool for navigating life’s ongoing challenges.
How is research evolving around Zoloft and postpartum treatment approaches?
Research on Zoloft and postpartum care is evolving in promising directions, especially with the emergence of precision psychiatry. Genetic testing, for instance, is being explored to predict which women may respond best to Zoloft versus other SSRIs. Meanwhile, studies are examining how Zoloft might be paired with novel digital health tools, such as app-based CBT programs tailored for postpartum mothers. There’s also growing interest in the drug’s effects on neuroplasticity—how it may support the brain’s ability to adapt and rewire itself after periods of emotional trauma. New clinical trials are investigating whether early intervention with Zoloft can prevent chronic mood disorders in high-risk populations. These developments point to a future where treatment is more personalized, data-driven, and accessible than ever before.
Conclusion: Reclaiming Well-Being with Zoloft and Informed Empowerment
For countless women navigating the emotional labyrinth of new motherhood, the path to healing can feel elusive, especially when anxiety overshadows joy and connection. In such moments, understanding the value of treatments like Zoloft becomes not only a clinical consideration but an act of self-preservation. This article has offered breakthrough insights on Zoloft for postpartum anxiety: what every new mom should know, emphasizing not only its pharmacological role but also its emotional and relational dimensions. From its ability to restore emotional equilibrium and improve quality of life to its compatibility with breastfeeding and therapy, Zoloft emerges as a viable and often transformative option for mothers facing postpartum anxiety and depression.
As with any medical decision, the choice to use Zoloft should be grounded in informed dialogue, self-reflection, and compassionate care. Mothers deserve access to treatments that honor both their vulnerability and their strength. They deserve support that addresses the full spectrum of their needs—not just symptom relief, but empowerment, validation, and sustained well-being. In reclaiming mental health with the aid of tools like Zoloft, new mothers are not simply surviving motherhood—they are reclaiming their capacity to flourish within it. The journey may be challenging, but it is navigable, and with the right support, it can lead to a place not just of recovery, but of renewed joy and self-trust.
Further Reading:
A Randomized, Placebo-Controlled, Double-Blind Trial of Sertraline for Postpartum Depression
Using sertraline in postpartum and breastfeeding: balancing risks and benefits



