Understanding the 4 cycles of period is more than just tracking menstruation—it’s about decoding the powerful hormonal patterns that influence not only reproductive function but also mental health, sexual wellness, and physical performance. These cycles, which include the menstrual, follicular, ovulatory, and luteal phases, orchestrate a symphony of changes across a woman’s body each month. For those navigating adulthood, especially college graduates managing health, relationships, and fertility choices, comprehending the 4 cycles of period can be a transformative key to better self-awareness, medical decision-making, and enhanced quality of life.
You may also like: The Vital Link Between Sex and Hormones During Menopause: What Every Woman Should Know
Why the 4 Menstrual Phases Matter for Overall Health
The menstrual cycle isn’t solely a reproductive event—it reflects a woman’s broader health status and biological rhythms. When balanced, it contributes to mood stability, metabolic consistency, sexual vitality, and even cognitive clarity. But when disrupted, it may signal underlying health issues like polycystic ovary syndrome (PCOS), endometriosis, or thyroid dysfunction.
The 4 menstrual phases—menstrual, follicular, ovulation, and luteal—serve as a framework for understanding these shifts. Each phase is driven by hormonal interplay, primarily involving estrogen, progesterone, follicle-stimulating hormone (FSH), and luteinizing hormone (LH). These hormones fluctuate with great precision and directly impact how one feels physically and emotionally.
Moreover, understanding the menstrual cycle hormone chart helps demystify these fluctuations. For example, estrogen surges before ovulation, boosting libido and energy, while progesterone dominates the luteal phase, often bringing calmness or, if imbalanced, premenstrual symptoms. This biological blueprint can guide choices in sexual activity, fertility planning, athletic training, and mental health support.

The Menstrual Phase: When the Cycle Begins
The first of the 4 stages of menstrual cycle is the menstrual phase, marked by the shedding of the uterine lining. It’s commonly known as the period, a visible and tangible manifestation of the reproductive cycle. For most women, this phase lasts between three to seven days, though it’s not unusual to experience variations. For instance, a 1 day period or one day menstrual flow may still be considered normal if it fits a person’s typical cycle pattern.
During this phase, estrogen and progesterone are at their lowest, which can lead to fatigue, lower mood, and decreased libido. These symptoms are not mere nuisances but reflections of hormonal withdrawal. However, some women may feel relief as bloating subsides and the body resets itself hormonally.
For those wondering how long can a period last or how long does a period last, the answer isn’t universally fixed. While the average duration is around five days, some experience a period 4 days early or period 5 days early, particularly under stress or during lifestyle changes. If menstruation starts and stops irregularly or drastically shortens, it’s valid to ask why would my period end early or does your period change dates. These occurrences often relate to shifting hormone levels, changes in body weight, travel, or underlying conditions, and they underscore the importance of body literacy.

Follicular Phase: A Time of Renewal and Growth
Following menstruation, the follicular phase begins. This second stage of the 4 stages of menstruation cycle is named for the follicle-stimulating hormone (FSH), which promotes the development of ovarian follicles—each containing an egg. Estrogen levels rise steadily, thickening the uterine lining in preparation for potential pregnancy.
The follicular phase is often associated with increased motivation, enhanced cognitive function, and better tolerance for physical exertion. Many women notice that during this time, they feel more productive, social, and even sexually inclined. These changes correspond with surging estrogen, which positively affects neurotransmitters like serotonin and dopamine.
For individuals tracking their cycle, this is often the most overlooked yet crucial phase. Not only does it bridge menstruation and ovulation, but it also sets the hormonal foundation for the rest of the month. If estrogen levels rise too slowly, ovulation may be delayed or skipped altogether, raising the question: can your period switch cycles or do your menstrual cycle change? Yes, it can—due to factors such as intense exercise, nutritional deficiencies, or medical conditions.
Understanding this phase allows for optimizing workouts, initiating new projects, or scheduling social engagements during a biologically high-functioning window. It’s also a great time to observe cervical fluid, as increasing estrogen leads to the appearance of clear, stretchy mucus—a sign that ovulation is approaching.

Ovulation: The Pinnacle of Fertility and Hormonal Energy
Ovulation is the briefest yet arguably most impactful of the 4 cycles of period. Occurring around day 14 of a 28-day cycle, this phase involves a surge in luteinizing hormone (LH), which triggers the release of a mature egg from the ovary. The window of fertility is narrow—only about 12 to 24 hours—but because sperm can survive up to five days, this fertile window extends a few days before and after ovulation.
Many women experience a spike in libido, subtle abdominal cramping (known as mittelschmerz), and heightened senses during this phase. These evolutionary advantages are no accident—they biologically prime the body for reproduction. For those trying to conceive, tracking ovulation is essential. For those avoiding pregnancy, understanding this window is equally critical, especially when using fertility awareness methods.
But ovulation isn’t just about fertility. It marks the hormonal high point of the cycle. Estrogen peaks, and testosterone—often overlooked in female health—also rises, boosting confidence, sexual desire, and muscle strength. These effects can be leveraged for athletic training, public speaking, or creative output.
Yet ovulation can also stir anxiety or agitation in some individuals, particularly if there are hormonal imbalances. Monitoring symptoms during this phase can provide insights into endocrine health and guide discussions with healthcare providers. For those wondering how do you know when your period is over, the days following ovulation often offer a reprieve from bleeding, but new hormonal shifts soon begin as the body transitions into the luteal phase.
Luteal Phase: Preparing for Potential Pregnancy—or the Next Cycle
The luteal phase follows ovulation and typically lasts 12 to 14 days. Progesterone, secreted by the corpus luteum (the follicle’s remnants), takes center stage. It stabilizes the uterine lining in anticipation of a fertilized egg. If implantation doesn’t occur, progesterone levels fall, triggering menstruation and beginning the cycle anew.
During this phase, many women encounter period symptoms such as bloating, mood swings, breast tenderness, and food cravings—collectively known as premenstrual syndrome (PMS). These changes are deeply tied to the hormonal flux of falling estrogen and rising, then dropping, progesterone. The luteal phase is a time of introspection and emotional sensitivity, offering a chance to reflect, retreat, and rest.
Understanding how you feel at different stages of menstrual cycle helps normalize these experiences and encourages self-compassion rather than self-criticism. If progesterone levels are too low, symptoms can be particularly intense, sometimes manifesting as premenstrual dysphoric disorder (PMDD), a condition that warrants clinical attention.
Women often ask, how long does a female period last, and it’s important to differentiate: the period itself is distinct from the luteal phase, though the two are closely linked. A normal luteal phase should remain fairly constant, but an abnormal duration might prompt concern about luteal phase deficiency, which can impact fertility and mood regulation.
The luteal phase also brings up the question, how do you know when your period is over? Biologically, menstruation ends when bleeding stops, but emotionally, it might not feel complete until the body transitions into the follicular phase again. The experience is holistic, encompassing more than just physical symptoms.

The 4 Cycles of Period and Sexual Health: Bridging Biology and Intimacy
Sexual health is intricately woven into the 4 phases of menstrual cycle. Libido fluctuates naturally with hormonal shifts. Estrogen and testosterone during the follicular and ovulatory phases amplify sexual desire, while progesterone in the luteal phase may either enhance intimacy through emotional closeness or reduce sexual interest depending on individual physiology.
Communication with partners about these shifts can foster healthier, more attuned relationships. For instance, knowing that irritability may stem from hormonal changes rather than interpersonal conflict can alleviate unnecessary tension. Likewise, planning romantic or sexual activities around high-libido phases can enhance satisfaction and connection.
Contraceptive decisions are also influenced by cycle understanding. For those relying on natural family planning, detailed knowledge of the menstrual period starts and stops becomes a cornerstone of success. Conversely, for individuals using hormonal birth control, recognizing how synthetic hormones override the natural rhythm of the 4 cycles of period can clarify side effects and empower informed consent.
Sexual health isn’t just about reproduction—it’s about autonomy, pleasure, and connection. Recognizing how cycle phases influence these dimensions can lead to more fulfilling, consensual, and empathetic sexual experiences.
The Science Behind Hormonal Fluctuations: A Closer Look at the Menstrual Cycle Hormone Chart
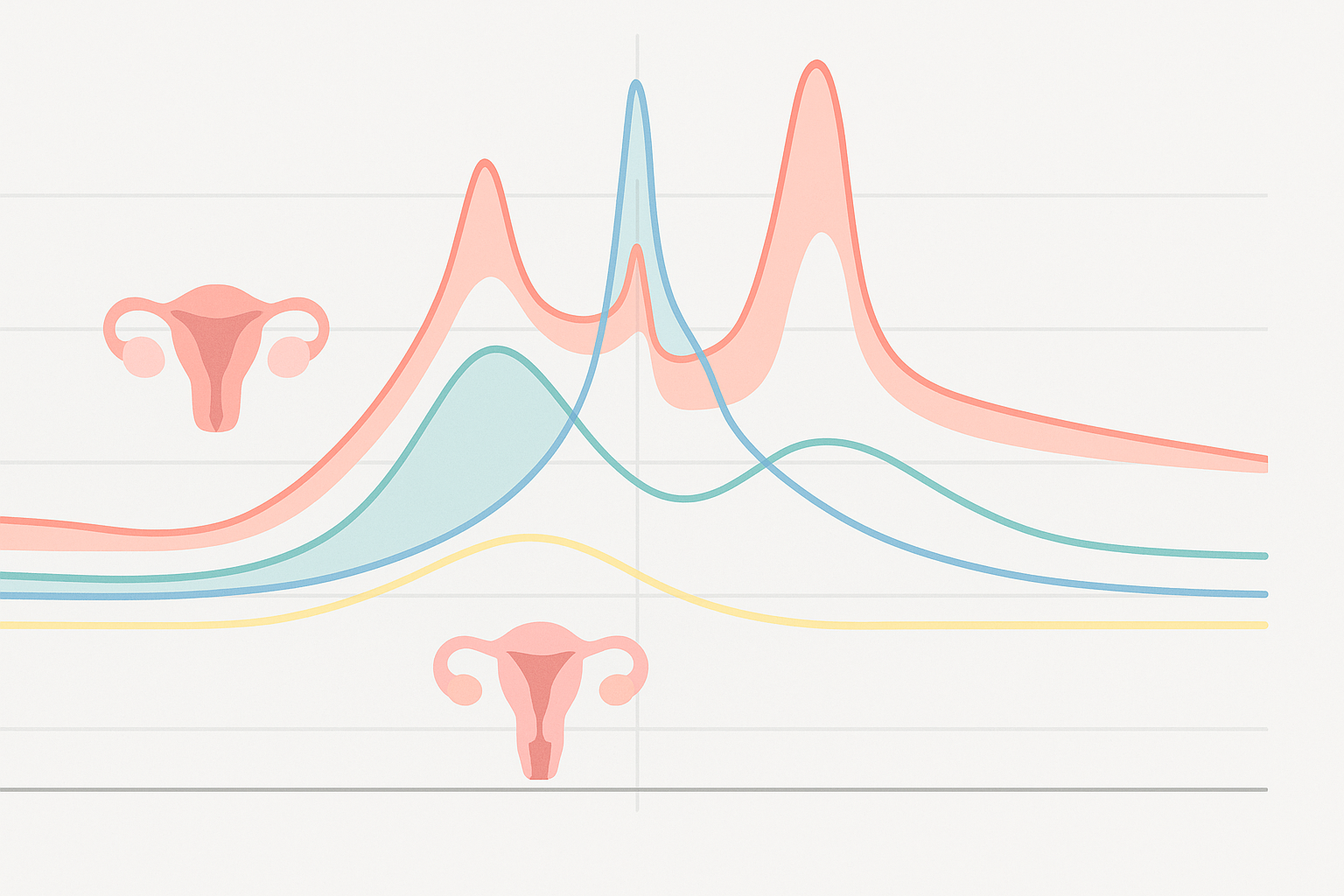
To truly understand the menstrual rhythm, the menstrual cycle hormone chart is an invaluable tool. This visual representation maps out the rise and fall of key hormones across the month, offering insights into why one feels differently week to week. FSH dominates early in the cycle, stimulating follicular growth. Estrogen climbs mid-cycle, facilitating ovulation. LH spikes abruptly to release the egg. Progesterone takes the lead post-ovulation, preparing the body for a potential pregnancy.
The dance of these hormones is both delicate and robust. Even minor imbalances can produce significant changes in mood, energy, sleep, and sexual function. This is why individuals may ask questions like how long is a period supposed to last, or what is considered last day of period. These aren’t just questions of convenience—they’re reflections of deeper hormonal literacy.
Hormone testing, especially for those with irregular cycles or severe PMS, can provide clarity. Healthcare professionals often recommend mid-luteal phase progesterone tests or day-3 estrogen and FSH levels to assess fertility status. While the chart may seem complex, even a basic understanding empowers one to advocate for their health more effectively.
What Are the Four Stages of the Menstrual Cycle and Why They Vary
Although the four stages of the menstrual cycle are generally predictable, they can shift over time or due to lifestyle and health factors. Stress, travel, illness, and medications can all influence hormone production. That’s why questions such as does your period change dates, or how long does a period last for a woman, remain relevant even for those with years of menstrual experience.
Significant life stages—such as puberty, postpartum, perimenopause, or starting/stopping hormonal contraception—can dramatically affect cycle regularity and symptom severity. Understanding that these fluctuations are biologically normal helps reduce anxiety and fosters a more compassionate approach to bodily changes.
Those experiencing abrupt changes, like a 1 day period or sudden cycle length variation, may wonder if this signals a deeper issue. While sometimes benign, such shifts can also suggest hormonal imbalances or medical conditions like PCOS, endometriosis, or thyroid dysfunction. Accurate tracking and open dialogue with healthcare providers can lead to better outcomes and earlier intervention when needed.
When to Seek Help: Irregularities, Symptoms, and Health Concerns
Though variation is common, there are instances when menstrual changes warrant medical attention. For example, if someone experiences a one day period that deviates from their usual flow for several months, or if menstrual cycle hormone charts reveal consistently abnormal levels, further evaluation is important. Heavy bleeding, intense pain, or emotional volatility can also indicate underlying issues.
Frequent cycle changes—such as a period 4 days early every month—can disrupt fertility planning, quality of life, and hormonal stability. Tools like symptom trackers, basal body temperature monitoring, and ovulation kits help provide a clearer picture. Armed with this data, healthcare providers can offer tailored treatment, whether through hormone therapy, lifestyle changes, or integrative approaches.
People also often ask, how can you tell when your period is over, or how do you know when your done with your period. These are not trivial curiosities. The end of menstruation is a biological milestone that marks the shift to a different hormonal profile. Tuning into this transition can help prevent confusion and optimize planning for activities, medications, or fertility awareness.
Embracing the 4 Cycles of Period as a Vital Framework for Self-Knowledge
The 4 cycles of period are more than reproductive markers—they are windows into the state of one’s hormonal ecosystem. By tuning into each phase—menstrual, follicular, ovulatory, and luteal—one can align decisions with their biology. This includes everything from adjusting workouts to managing relationships, optimizing work schedules, and practicing self-care.
Such knowledge fosters empowerment. No longer does one have to wonder when do period symptoms start, or feel blindsided by emotional swings. Instead, with tools like cycle charting and hormonal education, individuals can anticipate, adapt, and thrive. Whether dealing with a 1 day period, tracking a period 5 days early, or simply navigating the tides of sexual health, awareness offers agency.
And though cycles vary—sometimes leaving us wondering, can your period switch cycles, or do your menstrual cycle change—the underlying framework remains a reliable guide. It invites us to be in tune with our internal rhythm rather than at war with it.
Frequently Asked Questions About Navigating the 4 Cycles of Period and Menstrual Changes
1. How do the 4 stages of menstruation cycle impact your emotional resilience throughout the month?
The 4 stages of menstruation cycle—menstrual, follicular, ovulation, and luteal—deeply influence emotional processing, which can affect how you handle stress, conflict, or even decision-making. During the follicular phase, for example, rising estrogen often boosts mood and cognitive sharpness, making it a good time to tackle difficult tasks. Conversely, the luteal phase, which leads into menstruation, is when progesterone dominates and can cause increased emotional sensitivity or irritability. Understanding how you feel at different stages of menstrual cycle can help with emotional regulation and scheduling key responsibilities. Journaling your mood in alignment with the 4 menstrual phases can uncover patterns and empower better planning around personal and professional goals.
2. Why would my period end early, and is a one day period cause for concern?
A one day period or menstrual flow shorter than usual might not always indicate a health issue, but context matters. Lifestyle changes like increased physical activity, stress, or significant weight fluctuation can disrupt the normal rhythm of the 4 stages of menstrual cycle. In some cases, early termination of menstruation may signal hormonal imbalance, thyroid issues, or even early perimenopause. While a one day period occasionally isn’t uncommon, frequent episodes should prompt a review of the menstrual cycle hormone chart with a healthcare provider. Keep in mind that what is considered last day of period might vary depending on whether spotting continues beyond the heavy flow.
3. How long does a period last for a woman who is experiencing hormone fluctuations?
How long does a period last for a woman is influenced by factors like age, stress levels, medication, and underlying health conditions. For women with hormonal imbalances—especially those related to PCOS or thyroid dysfunction—the menstrual phase can be either shorter (e.g., a 1 day period) or excessively long. In some cases, the menstrual period starts and stops unpredictably across cycles. A healthy menstrual cycle generally reflects the integrity of all 4 phases of menstrual cycle, so any disruption to one stage—like a prolonged follicular phase—can impact the total duration of bleeding. Tracking changes over 4 cycles of period can reveal whether irregularities are isolated or part of a broader trend requiring attention.
4. How do you know when your period is over, especially when spotting persists?
How do you know when your period is over can depend on whether you’re referring to active bleeding or residual spotting. Light brown or pink discharge in the days following menstruation is common and may last up to two days. But what is considered last day of period often refers to the final day of red, consistent flow. If spotting continues intermittently, it may not signify a continuous period but rather delayed shedding or even breakthrough bleeding. Understanding the 4 stages of menstruation cycle helps determine whether spotting is normal or indicative of cycle disruption—especially if it occurs frequently outside the luteal phase.
5. Can your period switch cycles due to travel, stress, or lifestyle changes?
Yes, the menstrual cycle is sensitive to environmental and emotional shifts, so can your period switch cycles due to external factors? Absolutely. Travel, especially across time zones, can reset circadian rhythms and, in turn, hormonal patterns. Similarly, elevated cortisol levels from stress may inhibit ovulation, delaying or advancing the start of the next cycle. If you notice a period 4 days early or period 5 days early, assess lifestyle changes from the prior month. Tracking 4 cycles of period back-to-back can help identify whether the shift is temporary or part of a pattern. Sleep, nutrition, and stress management often help reestablish regularity.
6. When do period symptoms start in relation to the 4 phases of menstrual cycle?
When do period symptoms start depends on the individual and their sensitivity to hormonal changes, but symptoms often begin during the late luteal phase. This is when progesterone peaks and serotonin levels may decline, contributing to classic period symptoms like mood swings, bloating, and breast tenderness. For some, symptoms appear even earlier—before ovulation ends—especially if their hormonal transitions are abrupt. Understanding your own version of the 4 menstrual phases helps clarify when discomfort tends to emerge and why. Integrating mindfulness practices during the luteal stage can significantly reduce symptom severity over time.
7. How long can a period last and still be considered within normal range?
How long can a period last while remaining within clinical norms? Typically, 3 to 7 days is considered normal. However, if menstruation extends beyond 8 days or is consistently short—like a 1 day period—it could signal hormonal irregularities or uterine abnormalities like fibroids. The answer also depends on how your body moves through the 4 stages of menstrual cycle, as delays in endometrial shedding may extend the bleeding phase. It’s also important to distinguish between active flow and prolonged spotting, which may be misleading when evaluating cycle length. Repeated deviations across 4 cycles of period should prompt medical evaluation.
8. What does a menstrual cycle hormone chart reveal about your health?
A menstrual cycle hormone chart offers a visual breakdown of fluctuations in estrogen, progesterone, LH, and FSH across the 4 stages of menstruation cycle. By tracking hormone peaks and dips, it becomes easier to correlate symptoms with hormonal activity—like why you feel energized post-period but sluggish during PMS. This chart also provides valuable insight into whether ovulation is occurring regularly, which is crucial for both fertility and metabolic health. Over time, reviewing data across 4 cycles of period can help identify abnormalities such as anovulatory cycles or luteal phase defects. It’s an essential tool for anyone exploring hormonal birth control alternatives or managing PCOS.
9. How you feel at different stages of menstrual cycle: psychological and physical effects
How you feel at different stages of menstrual cycle is influenced by the dominant hormone of each phase. The follicular phase, dominated by estrogen, often brings improved cognitive clarity and social energy, while the luteal phase—governed by progesterone—can cause withdrawal and fatigue. Some women even report changes in how they interpret social cues or manage conflict based on the 4 menstrual phases. Recognizing how your behavior and mindset shift throughout the 4 stages of menstruation cycle can improve self-awareness and communication in both personal and professional settings. It’s also a valuable strategy in tailoring your diet and workouts to your cycle phase for better results.
10. Does your period change dates permanently, or can it fluctuate unpredictably?
Does your period change dates from time to time or permanently? Both are possible depending on your health status and hormonal stability. Occasional changes, such as a period 5 days early, might result from stress or illness, while permanent shifts often reflect long-term changes in hormone levels—like transitioning into perimenopause or recovering from childbirth. The key is to track the shift across 4 cycles of period to determine if it’s a trend. If irregularity persists and is accompanied by cycle phase disruption, it may point to underlying endocrine issues. Ultimately, while short-term deviations are normal, consistent changes merit professional evaluation to preserve reproductive health.
Conclusion: Honoring Hormonal Rhythms and Elevating Reproductive Health Awareness
Understanding the 4 cycles of period is not merely a biological study—it is an act of empowerment, self-respect, and health literacy. These four phases shape not only our reproductive capacity but also our energy, mood, creativity, and intimacy. When we honor this cycle, we gain the power to live more rhythmically and purposefully.
This journey begins with knowledge: knowing how long does a period last, recognizing the nuances of the menstrual cycle hormone chart, and discerning how do you know when your period is over. It extends into choices—about contraception, fertility, self-care, and relationships. And it culminates in ownership, where the cycle becomes not an inconvenience but a powerful signal from the body about its internal workings.
The 4 stages of menstruation cycle are universal, but their expression is personal. By embracing these patterns, tracking their signs, and seeking support when needed, every individual can cultivate a deeper connection with their body and enhance both reproductive and sexual health. Let this awareness be a foundation for health equity, informed choice, and lifelong vitality.
Further Reading:
Cycle Syncing: How to Understand Your Menstrual Cycle to Reduce Period Symptoms



